Clin Oral Investig:随机对照试验结果并不支持牙周手术过程中全身应用甲硝唑
2022-06-09 sunshine MedSci原创
牙周炎是一种慢性多因素的炎症性疾病,与菌斑生物膜失调有关,其特点是牙齿支持装置组织的逐步破坏。
牙周炎是一种慢性多因素的炎症性疾病,与菌斑生物膜失调有关,其特点是牙齿支持装置组织的逐步破坏。近日,发表于Clin Oral Investig的一项随机对照研究评估了在牙周手术中辅助甲硝唑的临床和微生物学影响。

研究纳入无系统性疾病的III-IV期B-C级牙周炎患者,在龈下机械性治疗后随机分配到接受甲硝唑或安慰剂辅助牙周手术。初次就诊时、龈下机械性治疗后6周,以及术后3、6和12个月时记录所有患者的临床变量。在初次和最后一次就诊时采集微生物样本,并通过定量聚合酶链反应进行分析。
结果显示,两个治疗组在初次和最后(1年)随访就诊时,探诊深度的减少没有统计学上的显著差异。此外,在比较龈下器械术后和最终就诊时,研究组之间没有统计学意义上的差异。然而,术后3个月,试验组的探诊深度(平均差异,MD = 0.31毫米,95%置信区间,CI [0.13; 0.49]; p = 0.001)和临床附着水平(MD = 0.64毫米,95% CI [0.02; 1.27]; p = 0.044)都较安慰剂组明显降低。
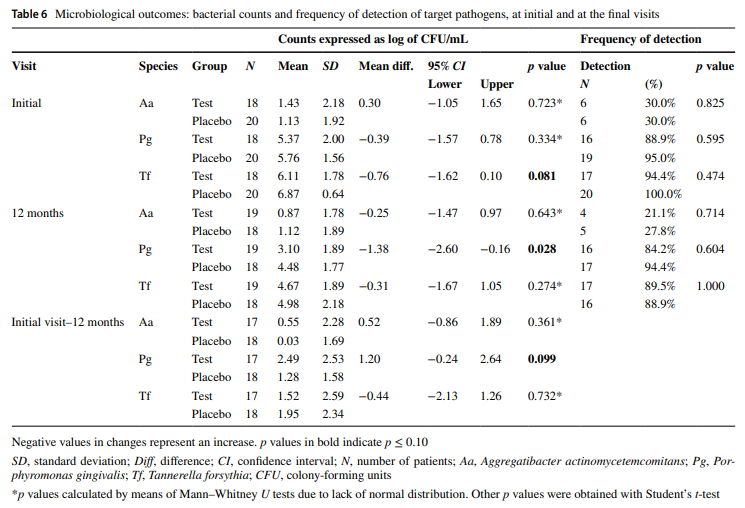
综上所述,该研究结果表明,在牙周手术中辅助全身使用甲硝唑对临床和微生物影响有限,因此,不推荐使用。目前还没有研究评估在牙周手术(牙周治疗的第3步)中辅助使用全身甲硝唑的临床和微生物学影响。但是,本研究的结果不支持在牙周手术中辅助使用全身性甲硝唑。
原始出处:
James Rudolph Collins, et al., Adjunctive efficacy of systemic metronidazole in the surgical treatment of periodontitis: a double-blind parallel randomized clinical trial. Clin Oral Investig. 2022 May;26(5):4195-4207. doi: 10.1007/s00784-022-04392-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oral#
50
#EST#
34
#对照试验#
44
#对照#
38
#随机对照试验#
46
#甲硝唑#
49
#牙周#
37