肺动脉高压患者右心室重构可预测治疗反应
2022-05-14 刘少飞 MedSci原创
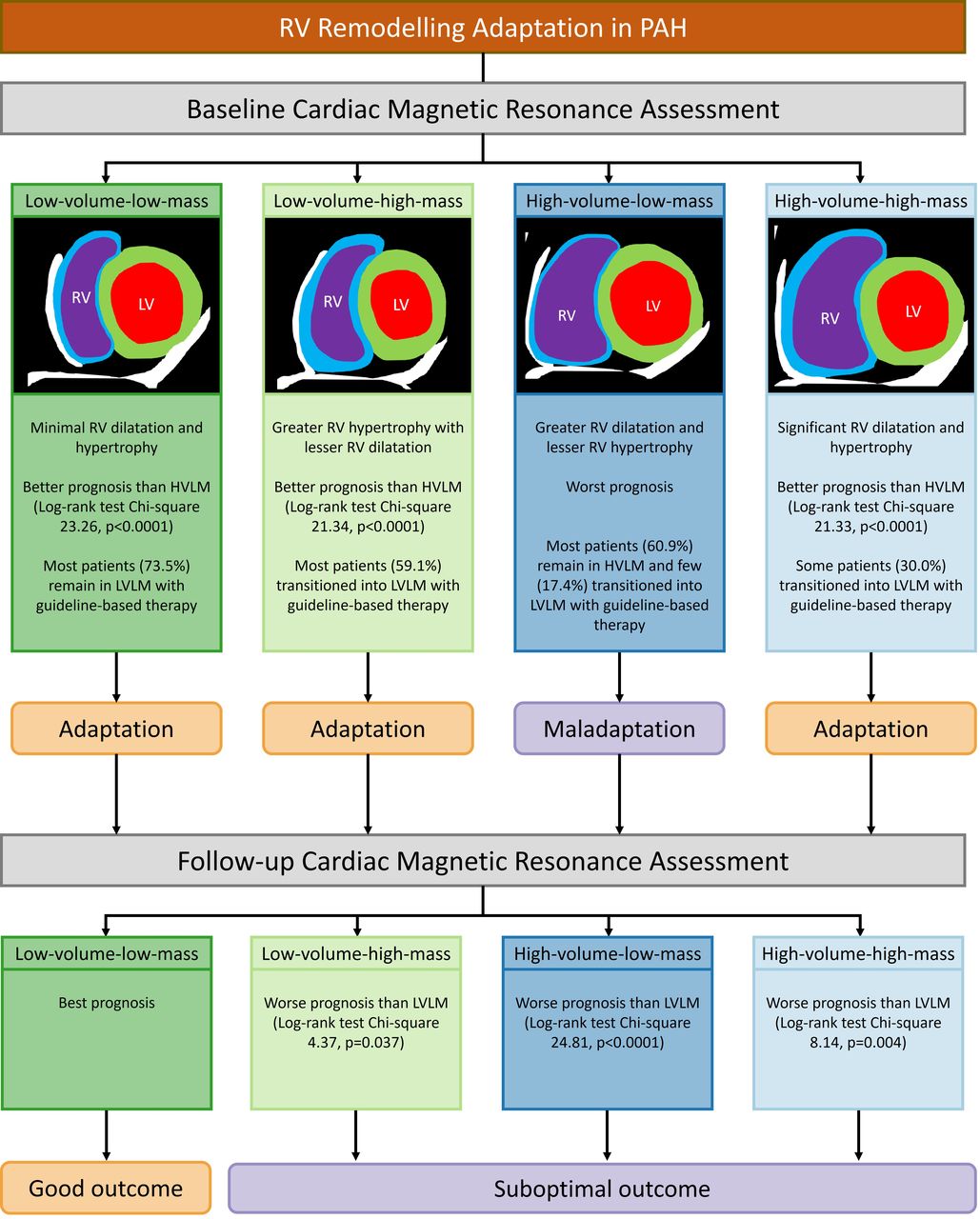
确定肺动脉高压 (PAH) 患者右心室适应模式的预后价值,在基线和随访时使用心脏磁共振 (CMR) 成像进行评估。
肺动脉高压 (PAH) 是一种缩短生命的疾病,其特征是影响肺小动脉的血管病变,导致后负荷增加且无需治疗右心室 (RV) 衰竭。评估疾病严重程度和预后对于选择治疗方案、肺移植时机和咨询患者至关重要。心脏磁共振 (CMR) 提供了对心室形态和功能的准确且可重复的评估。以前的研究使用 CMR 评估了 PAH 患者 RV 质量与体积之比的预后价值。在临床表现、血流动力学状态和存活率方面,低 RV 质量体积比(偏心性肥大)的患者被认为比 RV 质量体积比高(向心性肥大)的患者疾病更严重。
然而,低 RV 质量体积比在识别高危患者时可能不是最佳选择,因为它表明 RV 正常或由于偏心肥大而扩张。使用 CMR 评估 PAH 患者 RV 形态的更近期和更详细的方法是通过 RV 体积/质量分组,其中 RV 形态基于 RV 体积和质量阈值进行分类。
本研究的目的是使用 RV 体积/质量分组基于 RV 适应模式来表征 PAH 患者,评估治疗前的 RV 适应是否预测 PAH 治疗后逆转重塑的可能性,并评估重塑对预后的影响。
研究方法:
将在谢菲尔德肺血管疾病科就诊的疑似肺动脉高压患者纳入 ASPIRE(评估在转诊中心确定的肺动脉高压谱)登记处。在排除先天性心脏病的情况下,对连续患有 PAH 的患者进行随访,直至人口普查或死亡之日。根据年龄和性别调整的右心室收缩末期容积指数和心室质量指数用于将患者分为四个不同的容积/质量组:低容量-低质量、低容量-高质量、高容量-低- 质量和高容量 - 高质量。使用单因素方差分析和 Kaplan-Meier 图评估各组的预后价值。
研究结果:
共发现肺动脉高压患者505例,随访时死亡239例(47.3%)(中位4.85年,IQR 4.05)。患者的平均年龄为 59±16 岁,其中 161 名(32.7%)为男性。低容量低质量与 CMR 和右心导管插入指标相关,可预测预后改善。有 124 名患者接受了 CMR 随访(中位数 1.11 年,IQR 0.78)。在基线和随访中,高容量低肿块组的预后比低容量低肿块组更差(p<0.001)。PAH 治疗后,73.5% 的低容量-低质量患者仍留在该组中,而只有 17.4% 的高容量-低质量患者转变为低容量-低质量。
研究结论:
CMR 识别出具有低 RV 体积和质量的 PAH 患者,这些患者能够很好地适应增加的 RV 后负荷并具有低死亡率,以及具有高 RV 体积和低 RV 质量的患者代表适应不良和高死亡率。应将随访时的低 RV 体积和质量作为治疗目标。对于右室容积大而右室质量低的患者,可能早在诊断时就应考虑加强治疗。具有适应不良重塑(大体积-低质量)的患者处于治疗失败的高风险中。
参考文献:
Goh ZM, Balasubramanian N, Alabed S, Dwivedi K, Shahin Y, Rothman AMK, Garg P, Lawrie A, Capener D, Thompson AAR, Alandejani F, Wild JM, Johns CS, Lewis RA, Gosling R, Sharkey M, Condliffe R, Kiely DG, Swift AJ. Right ventricular remodelling in pulmonary arterial hypertension predicts treatment response. Heart. 2022 May 5:heartjnl-2021-320733. doi: 10.1136/heartjnl-2021-320733. Epub ahead of print. PMID: 35512982.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉高压#
27
#肺动脉高压患者#
38
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
58
好
48
#心室重构#
31
#右心室#
46