JAMA Intern Med:台湾学者发现慢阻肺患者起始应用支气管扩张剂30天内心血管病风险增加,
2018-01-04 许菁 中国循环杂志
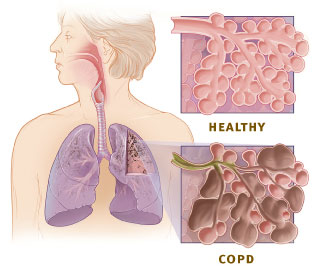
我国台湾学者发现,COPD患者在起始应用长效β2受体阻滞剂或者长效毒蕈碱拮抗剂的30天内,其心血管病包括冠心病、心律失常、心力衰竭或缺血性中风的风险大约增加50%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#支气管扩张剂#
38
#扩张#
38
#30天#
29
#血管病#
0
#支气管#
35
#Med#
18
学习了.不错
58