IBD: 生物和小分子双重疗法在治疗难治性小儿炎症性肠病中的作用
2020-11-07 MedSci原创 MedSci原创
抗肿瘤坏死因子单克隆抗体被批准用于治疗中度至重度小儿克罗恩病(CD)和溃疡性结肠炎(UC)。
抗肿瘤坏死因子-α(anti-TNF-α)单克隆抗体被批准用于治疗中度至重度小儿克罗恩病(CD)和溃疡性结肠炎(UC),但是小儿炎症性肠病(IBD)患者中,一线抗TNF-α治疗具有约40%的持久缓解率。三分之一的患者是抗TNF-α治疗的原发性无反应者,而改用其他抗TNF-α治疗的患者则更不可能产生临床反应。Vedolizumab(一种α4β7整联蛋白拮抗剂)和ustekinumab(一种抑制白介素(IL)-12和IL-23的人类单克隆抗体)在儿童中经常作为第二线生物制剂使用,但超过三分之一的儿童未能使用1年后达到无类固醇的临床缓解。Tofacitinib是一种口服小分子优先性janus激酶(JAK)1和JAK3抑制剂,是最新的疗法,已被证明可有效诱导和维持中度至重度UC成人的缓解。对于难于生物治疗的IBD患者,双重生物制剂或同时使用JAK抑制剂的生物制剂可能是一种治疗选择。目前,成人和小儿IBD患者关于双重生物疗法的疗效和安全性的数据非常有限。因此,本项研究旨在评估在难治性小儿IBD人群中同时使用两种生物疗法或生物与托法替尼联合治疗的有效性和安全性。

研究人员对正在进行的针对小儿IBD患者(小于18岁)治疗结局的单中心观察性队列研究收集了接受双重治疗的患者的数据。主要结局为6个月无类固醇缓解。次要结果包括基线至6个月之间无类固醇缓解的时间,血清生物标志物(C反应蛋白和红细胞沉降率)和白蛋白的变化以及不良事件。
结果显示:16名IBD儿童纳入本项研究(9例溃疡性结肠炎/ IBD未定,克罗恩病7例),病程平均为3(2.1-5.0)岁,在≥2种生物疗法失败后,所有患者在平均15.9(13.5-16.8)岁时开始了双重治疗。vedolizumab / tofacitinib治疗9例(56%),ustekinumab / vedolizumab治疗4例(25%),ustekinumab / tofacitinib治疗3例(19%);有 7例溃疡性结肠炎/ IBD未定,5例克罗恩病患者在6个月时持续无类固醇缓解。在基线和6个月之间,红细胞沉降率和C反应蛋白降低(分别为P = 0.021和P = 0.015),白蛋白升高(P = 0.003)。
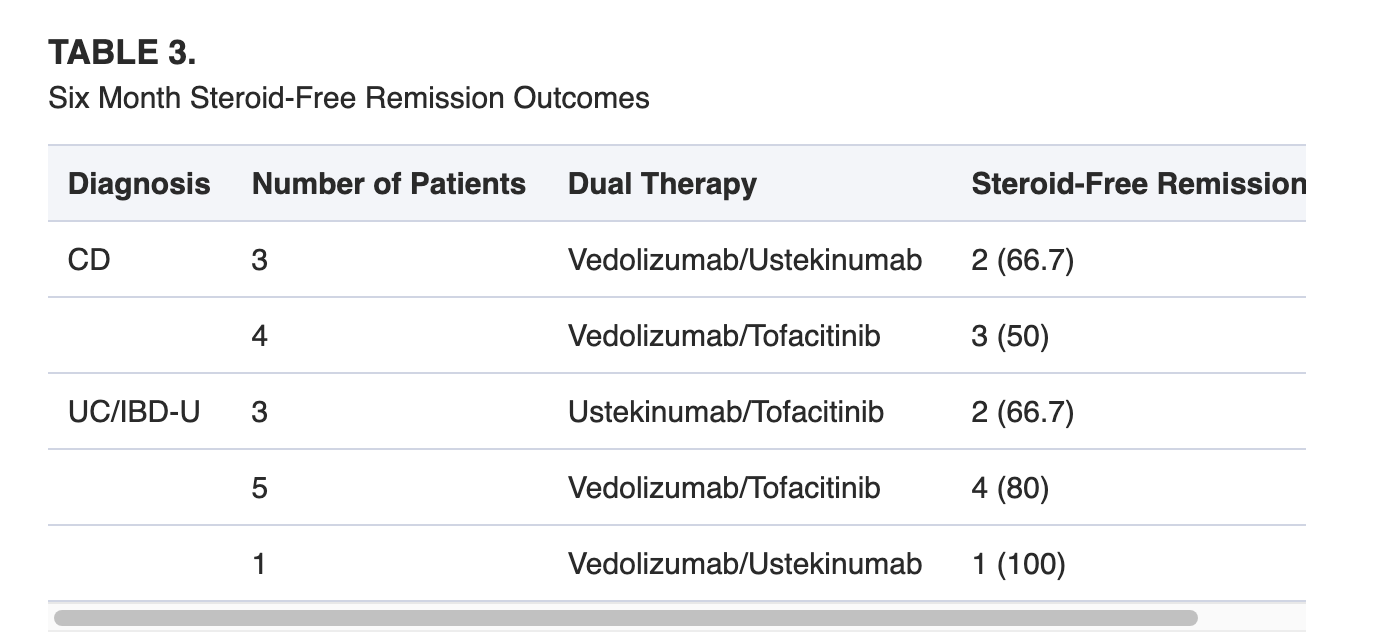
最后研究人员说道对于剩余治疗选择有限的患者,双重治疗可能是一种选择。它在本项试验中被证明是有效的。
原始出处:
Michael T Dolinger. Et al. Dual Biologic and Small Molecule Therapy for the Treatment of Refractory Pediatric Inflammatory Bowel Disease. Inflammatory Bowel Diseases.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#小分子#
38
#IBD#
40
#难治性#
29
#炎症性#
33