JACC:致病变异对非缺血性扩张型心肌病患者预后的影响
2021-10-26 Nebula MedSci原创
携带致病性或可能致病性变异的DCM患者比不携带致病/可能致病性突变的患者的预后要差
非缺血性扩张型心肌病 (DCM) 的特征是不可归因于异常负荷条件或冠状动脉疾病的左心室扩大和收缩功能障碍。DCM的人口患病率估计为 1/250-1/2500,是年轻人心力衰竭的最常见原因,也是全球心脏移植的主要原因。DCM是室性心律失常的常见原因,与较高的心源性猝死 (SCD) 风险相关。
迄今为止,DCM患者的遗传变异与其临床预后的相关性尚未明确。本研究旨在评估DCM患者的致病性基因变异的预后影响。
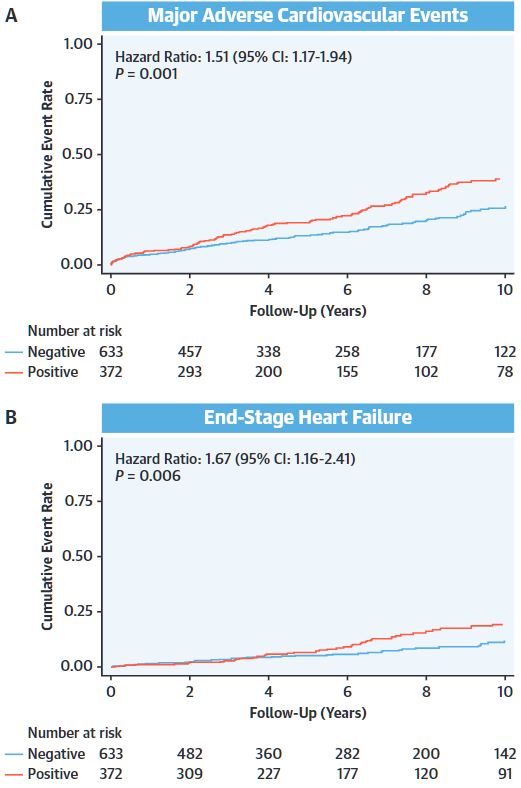
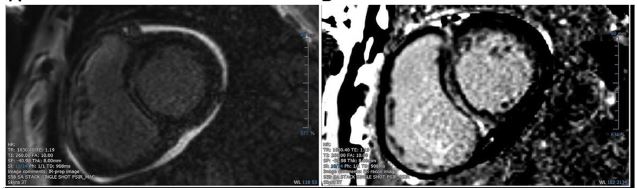
研究人员从20个中心回顾性地收集了1005位基因型明确的DCM先证者的基线和纵向临床数据。372位(37%)患者携带致病性或可能致病性变异(基因型阳性),633位(63%)患者为基因型阴性。主要终点是主要不良心血管事件。次要终点是终末期心力衰竭(ESHF)、恶性室性心律失常(MVA)和左心室逆向重构(LVRR)。
两组患者主要不良心血管事件和终末心衰的累积发生率
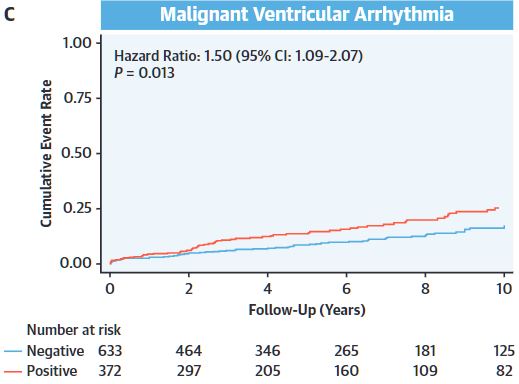
中位随访了4.04年(四分位范围 1.70-7.50年)后,基因型阳性组有118位(31.7%)患者发生了主要终点事件,而基因型阴性组有125位(19.8%)发生了主要终点事件(风险比[HR] 1.51, 95% CI 1.17-1.94; p=0.001)。60位(15.1%)基因型阳性患者和55位(8.7%)基因型阴性患者发生了ESHF(HR 1.67, 95% CI 1.16-2.41; p=0.006)。73位(19.6%)基因型阳性患者和77位(12.2%)基因型阴性患者发生了MVA(HR 1.50, 95% CI 1.09-2.07; p=0.013)。
两组患者恶性室性心律失常的累积发生率
此外,39.6%的基因型阳性患者和46.2%的基因型阴性患者发生了LVRR(p=0.047)。在基线左心室射血分数≤35%的个体中,与基因型阴性的同龄人相比,基因型阳性患者发生了更多的主要不良心血管事件、EFHF和MVA(p<0.02)。最后,LVRR和临床结局都会因潜在的变异基因而异。
综上所述,在该研究中,携带致病性或可能致病性变异的DCM患者比不携带致病/可能致病性突变的患者的预后要差。携带不同的基因变异对预后的影响也会有所不同。
原始出处:
Escobar-Lopez Luis,Ochoa Juan Pablo,Mirelis Jesús G et al. Association of Genetic Variants With Outcomes in Patients With Nonischemic Dilated Cardiomyopathy.[J] .J Am Coll Cardiol, 2021, 78: 1682-1699.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#患者预后#
0
#扩张#
34
#缺血性#
0
#JACC#
22
#ACC#
0
#变异#
18
#肌病#
26