Diabetologia:亚裔印度人年轻发病的糖尿病与测量和遗传决定的β细胞功能降低有关
2022-03-23 从医路漫漫 MedSci原创
糖尿病患病率正在上升,这是南亚发病率的主要负担。国际糖尿病联合会预测,到2045年,将有1.514亿南亚土著人患有2型糖尿病,几乎是目前患病率的两倍。
背景:糖尿病患病率正在上升,这是南亚发病率的主要负担。国际糖尿病联合会预测,到2045年,将有1.514亿南亚土著人患有2型糖尿病,几乎是目前患病率的两倍。一项大规模的人口调查,印度医学研究理事会-印度糖尿病(ICMRINDIAB)研究报告称,印度糖尿病的平均患病率为7.3%,各国之间差异很大。这高于苏格兰目前的患病率(6.3%),根据国际糖尿病联合会的估计,苏格兰是具有代表性的欧洲白人人口,或者欧洲大部分地区。南亚人的2型糖尿病是一个全球性的问题,因为他们构成了西方国家侨民的重要组成部分。据报道,生活在高收入国家的南亚人被诊断出糖尿病的时间比欧洲白人早5到10年。为了减轻全球糖尿病的负担,有必要更好地描述这一族群中糖尿病的特定代谢和生理驱动因素。
亚裔印第安人的代谢表型与白人明显不同。由Yajnik和Yudkin进行的相对双能量X射线吸收扫描最好地捕捉到了“瘦胖”印度人的表型。这种表型表现为躯干脂肪增加,尽管BMI正常或较低,这与高胰岛素血症和其他胰岛素抵抗指标有关,从出生、儿童到成年都可以看到。许多研究已经调查了这种瘦脂肪表型与糖尿病风险的关系。到目前为止,大规模研究的重点是生活在高收入国家的南亚移民人口。其中,值得注意的是两项跨种族的比较研究。SABRE研究是一项前瞻性队列研究,比较了居住在英国的白人、亚裔印度人和非洲加勒比人族群患糖尿病的风险和与风险相关的变量。他们发现,与欧洲白人相比,在20年的随访期内发展为糖尿病的亚裔印度男性的BMI更低,腰臀比更高,躯干皮褶厚度更高,胰岛素抵抗更高,β细胞功能增强(代偿性),但在血脂方面没有差异。此外,英国生物库的一项分析表明,与体重指数>30公斤/平方米的白人参与者具有相同的糖尿病风险,南亚参与者的相当体重指数仅为22公斤/平方米
虽然已经确定,亚洲印度人的2型糖尿病的特点是发病年龄较早,BMI相对较低或更低,但尚未开展大规模研究,全面描述患有2型糖尿病的年轻、苗条的亚洲印度人的代谢表型和遗传风险。在跨种族的糖尿病比较研究中的一个主要挑战是缺乏可用于克服在比较来自不同地理卫生环境的临床措施时引入的偏见的遗传资源。印度-苏格兰糖尿病精确医学伙伴关系(INSIGNAL)汇集了印度和苏格兰(英国)糖尿病研究的数据资源。据我们所知,这项研究是第一项使用种族特定肥胖阈值在亚裔印度队列中全面了解年轻发病糖尿病的代谢风险因素的人群研究。然后,我们使用临床数据和由于β细胞功能受损而导致的2型糖尿病易感性的分区或特定过程多基因评分(PPS),检验了亚洲印度人年轻起病糖尿病的表型是β细胞缺陷的假设。
目的:南亚人,特别是亚裔印度人,与欧洲白人相比,患2型糖尿病的风险更高,而且发病年龄更早。发病年龄较早的原因与肥胖、β细胞功能和胰岛素敏感性的关系还没有得到充分的探讨。
方法:使用两个亚裔印度人队列,ICMR-INDIAB队列(印度医学研究理事会-印度糖尿病研究)和DMDSC队列(Mohan博士的糖尿病专科中心),以及一名欧洲白人,ESDC(东苏格兰糖尿病队列)。使用横断面设计,我们检查了健康、超重和肥胖的年轻糖尿病患者的相对患病率,根据他们的BMI进行了分类。我们探讨了临床测量的β细胞功能在亚裔印度人糖尿病发病中的作用。最后,对由于胰岛细胞功能低下而导致的糖尿病风险的分区多基因评分(PPS)的比较分布进行了检验。利用英国生物库的数据,试图复制这些基因发现。
结果:BMI正常的年轻发病糖尿病在欧洲白人中的患病率为9.3%,在亚裔印度人中为24%-39%。在年轻起病的亚洲印度人中,在调整了2型糖尿病家族史、性别、胰岛素敏感性和高密度脂蛋白-胆固醇后,瘦人比肥胖者刺激的C肽低492pmoL/ml(IQR353-616,p<0.0001)。在我们的研究中,亚裔印度人和来自英国生物库的南亚人比欧洲白人有更多的风险等位基因。在对β细胞功能的PPS进行加权后,亚裔印度人在遗传上决定的β细胞功能低于欧洲白人(p<0.0001)。在亚裔印度人中,PPS与诊断年龄有关,而在欧洲白人中则不相关。在BMI正常或被归类为超重和肥胖的亚裔印度人中,PPS分别解释了临床测量的β细胞功能变异的2%和糖尿病年龄变异的1.2%、0.97%和0.36%。
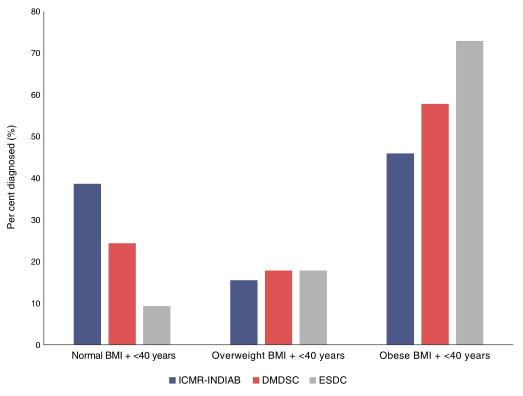
图1亚洲印度人(蓝色,ICMR-INDIAB队列;红色,DMDSC队列)和欧洲白人(灰色,ESDC队列)早发性糖尿病患者在每个BMI类别中的比例条形图。亚裔印度人的正常BMI<23 kg/m2,超重定义为BMI 23-25 kg/m2,体重指数>25 kg/m2。欧洲白人人群的正常BMI<25 kg/m2;超重定义为BMI 25-30 kg/m2,肥胖定义为BMI>30 kg/m2[。这两个种族的早发性被定义为40岁或更年轻(<40岁)的患者。

表1被诊断为年轻和年长的亚裔印度人的特征比较
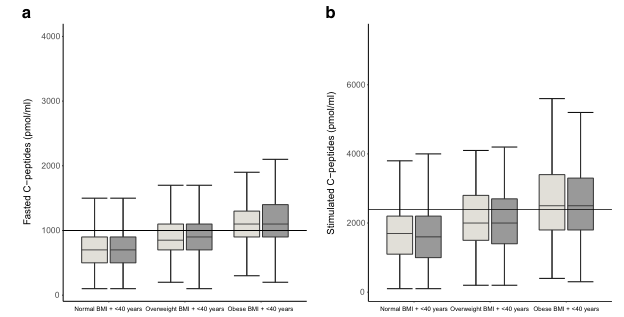
图2按BMI分类显示较低的空腹C肽水平(A)和刺激的C肽水平(B)的框图。所显示的数据来自患有2型糖尿病的亚洲印度人的DMDSC队列。亚裔印度人的正常BMI<23 kg/m2,超重定义为BMI 23-25 kg/m2,肥胖定义为BMI>25 kg/m2。早发的定义是那些在40岁或更年轻(<40岁)确诊的人。浅灰色,男性参与者;深灰色,女性参与者。与被归类为超重和肥胖者相比,体重指数正常的人空腹和刺激的C肽水平较低,β细胞功能也较低,胰岛素敏感性也有代偿性增加。在调整胰岛素敏感性后,刺激的C-肽水平与确诊年龄之间的关联仍然显著(p<0.0001)。
结论:年轻发病的糖尿病患者的瘦体重指数在亚裔印度人中的患病率是欧洲白人的两倍多。这种苗条的年轻发病糖尿病的表型似乎部分是由较低的β细胞功能驱动的。我们证明,患有糖尿病的亚裔印度人也具有较低的遗传决定的β细胞功能。
原文出处:Siddiqui MK, Anjana RM, Dawed AY,et al.Young-onset diabetes in Asian Indians is associated with lower measured and genetically determined beta cell function.Diabetologia 2022 Mar 05
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#β细胞功能#
44
#DIA#
45
#BET#
52
#细胞功能#
46
#β细胞#
54