Hypertension:高血压儿童和青少年尿酸水平与执行能力相关
2021-03-29 MedSci原创 MedSci原创
研究人员发现伴有原发性高血压风险的儿童血清尿酸水平与较差的执行能力呈正相关。通过纵向研究扩展这些横断面结果可能有助于明确高尿酸水平是否会增加青年人认知下降的风险。
观察性研究结果表明血清尿酸水平与心脏代谢危险因素和亚临床靶器官损害相关。

近日,心血管权威杂志Hypertension上发表了一篇研究文章,该研究旨在调查传统的心脏代谢危险因素和尿酸与儿童和青少年执行能力之间的关系。
研究人员纳入了评估原发性高血压5岁至18岁的儿童和青少年,并评估了他们传统的心脏代谢危险因素、尿酸和动态血压参数。执行能力由经过验证的执行功能行为评估量表父母问卷进行评估。
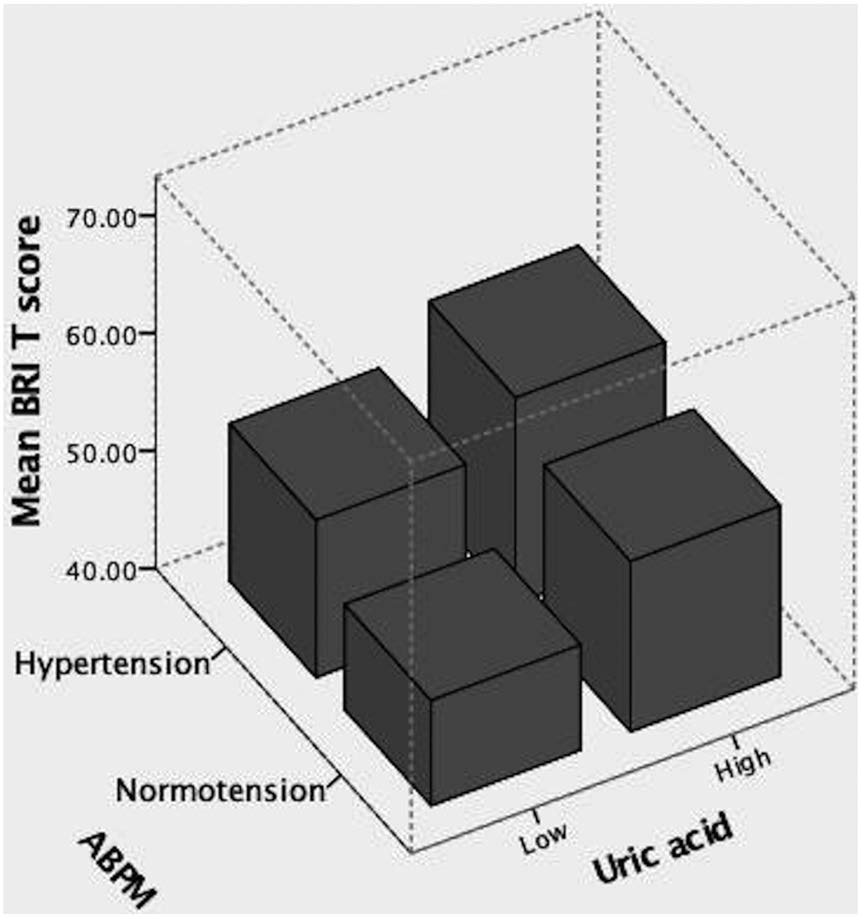
研究人员发现血清尿酸水平与心脏代谢参数、白天和夜间收缩压相关。高尿酸水平和动态性高血压与行为调节相关,而与其他心脏代谢危险因素或代谢综合征无关。合并高血压和高尿酸血症参与者具有最低的行为调节能力。高尿酸儿童的行为调节指数T评分较差,估计的临界平均值为56.47(95%CI为51.68-61.27),而低尿酸水平的儿童为49.22(95%CI为45.91-52.53)(P=0.023,根据年龄、性别、夜间收缩压、白天和夜间心率进行调整后)。介导分析表明,高尿酸水平对行为调节的部分影响是由夜间收缩压所介导。
总之,研究人员发现伴有原发性高血压风险的儿童血清尿酸水平与较差的执行能力呈正相关。通过纵向研究扩展这些横断面结果可能有助于明确高尿酸水平是否会增加青年人认知下降的风险。
原始出处:
Yun Gi Kim.et al.Different Influence of Blood Pressure on New-Onset Atrial Fibrillation in Pre- and Postmenopausal Women A Nationwide Population-Based Study.Hypertension.2021.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.16513
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#儿童和青少年#
46
#TENS#
0
#PE#
51
#Hypertension#
46