PLOS Pathog:发现一种抗病毒蛋白可能阻止黑猩猩传播HIV前体
2017-12-22 佚名 medicalxpress
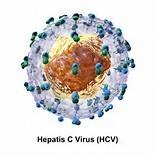
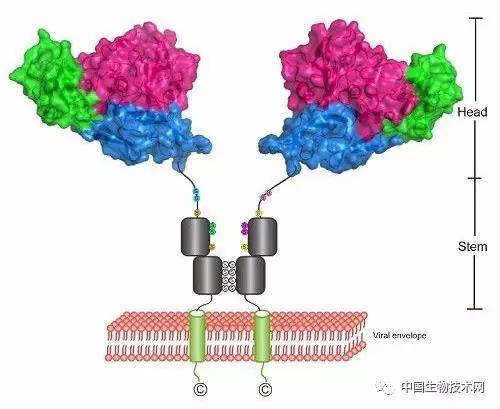
在人类中,被称为APOBEC3H的抗病毒蛋白质可以抵抗产生HIV-1的病毒的黑猩猩的跨物种传播。德国杜塞尔多夫海因里希 - 海涅大学的Zeli Zhang及其同事在一项新的PLOS病原体研究中介绍了这一发现。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#黑猩猩#
33
#病毒蛋白#
30
#抗病毒蛋白#
34
签到学习了
66
签到学习了--
71
签到学习了--
81
签到学习了--
59
签到学习了--
71
签到学习了--
27
签到学习了--
29