BMJ:关注早产儿神经发育,积极制定预防干预措施
2021-04-30 MedSci原创 MedSci原创
该研究报告了5岁半时的发育情况,包括对教育援助的需求,复杂的发展干预,以及父母对孩子发展的关注。每个胎龄组中严重/中度神经发育障碍的发生率仍然很高。

早产儿童可能经历许多发育困难,从严重到轻微的损害。这些缺陷大多在2岁以后被更好地识别出来,此时高层次的认知、语言和行为过程发展并影响早期的感觉运动能力。儿童早期神经发育障碍通常被报道为脑瘫、感觉和认知障碍的复合结果。更细微的缺陷,如行为困难或发育协调障碍,通常单独报告,它们可能改变儿童的社会情绪能力,影响日常活动和学校成绩,扰乱家庭功能,并需要大量的医疗、社会、教育和家庭支持。因此,所有的条件一起考虑是很重要的。此外,越来越多的人认为,父母的观点对于帮助弥合父母想要的结果信息和传统上提供给他们的信息之间的差距至关重要。
围产期重症监护的进展,包括产前糖皮质激素、外源性表面活性剂、无创呼吸支持、避免在出生后自由使用糖皮质激素治疗支气管肺发育不良,可提高早产婴儿的存活率,特别是那些极度早产(24-26周)的婴儿。最近以大量人口为基础的研究报告了儿童早期的结果,主要集中在那些极度早产的人身上。这组患者的长期预后没有令人信服的改善。非常早产(27-31周)或中度早产(32-34周)的婴儿产生的研究较少,但护理方面的变化也对这些婴儿产生了重大影响,他们在面临发育困难的婴儿中所占比例更大。因此,最新数据对于评估他们的需求和向利益相关者提供有用的信息至关重要。
EPIPAGE-2队列是2011年法国关于研究低于35周出生的孩子的一个国家的群体调查。在研究已经证明2岁时的生存率、新生儿预后和神经感觉障碍的改善。随后对5岁半时进行了评估。Véronique Pierrat等在BMJ发表研究文章,研究的目的是描述神经发育结果,包括脑瘫,感觉障碍,认知,行为困难和发育协调障碍,纳入EPIPAGE-2随访的儿童,以当代出生的早产儿为参考。为了进一步评估早产的家庭和社会负担,还报告了教育援助,使用复杂的发展干预和父母对发展的关注。
研究对象是在24-26周、27-31周和32-34周出生的4441名5岁半的儿童。主要观察指标为重度/中度神经发育障碍,定义为重度/中度脑瘫(大运动功能分类系统(GMFCS)≥2),或单侧或双侧失明或失聪,或完整的智商小于负两个标准差(韦氏学前和小学智力量表,第4版)。
轻度神经发育障碍,定义为轻度脑性麻痹(GMFCS-1),或视力残疾≥3.2/10和<5/10,或听力损失<40 dB,或全量表智商(-2到-1个标准差)或发育协调障碍(儿童运动评估量表,第二版,总分小于或等于第五百分位)、行为困难(强项及困难问卷,总分大于或等于第90百分位)、学校协助(有支持的主流班级或特殊学校)、复杂发展干预措施、家长对发展的关注。以当代出生儿童的得分分布为参考。
在4441名参与者中,3083名儿童(69.4%)接受了评估。
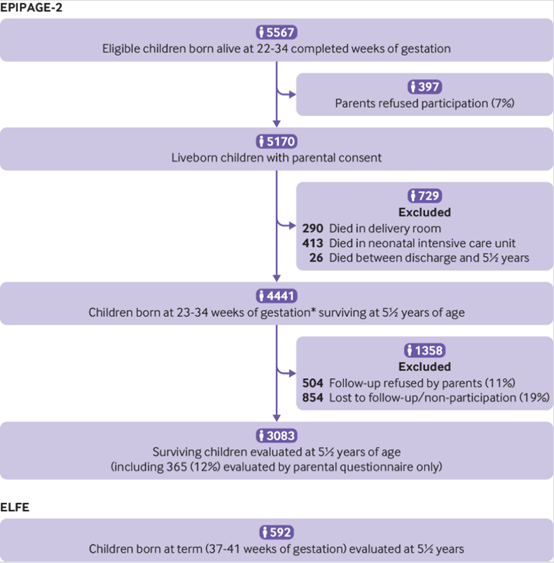
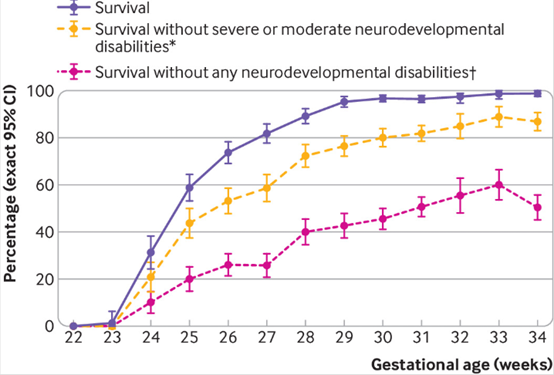
在EPIPAGE-2研究中,早产儿的5年半生存率、无严重/中度神经发育障碍生存率和无任何神经发育障碍的出生周生存率。为研究设计
和应答者选择校正的数据,*严重或中度脑瘫(大运动功能分类系统2-5级)、视力(双侧双眼视力<3.2/10)、听力(单侧-双侧听力损失≥40db未矫正或使用助听器部分矫正)、和全面智商低于两个标准差低于参考样本的均值足月出生的。†不包含脑瘫,没有视觉或听觉障碍,全面智商大于或等于一个标准差低于均值,不发展协调障碍,没有行为困难。
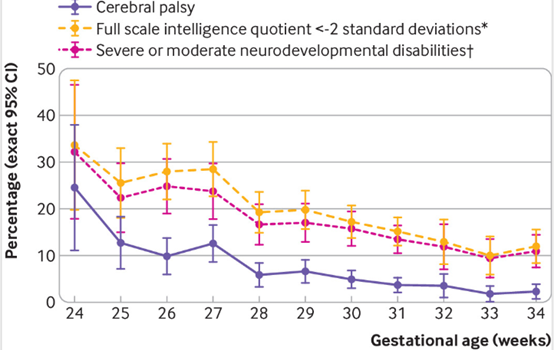
EPIPAGE-2研究中幸存者5年半时按孕周计算的结果。为研究设计和应答者选择校正的数据。*全量表智商小于负两个标准差,与足月出生的参考样本(37-41周)有关的分布截止点;†重度或中度脑瘫(大运动功能分类系统2-5级),视力(双侧双眼视力<3.2/10),听力(单侧-双侧听力损失≥40 dB,未矫正或使用助听器部分矫正),全量表智商低于足月出生参考样本均值两个标准差以下。
在24 – 26周,27-31周,32-34周严重/中度神经发育障碍发病率分别为28%(95%置信区间为23.4%-32.2%),19%(16.8%-20.7%)和12%(9.2%-14.0%);轻度障碍发病率为38.5%(33.7%-43.4%),36%(33.4%-38.1%)和34%(30.2%-37.4%)。在24-26周、27-31周和32-34周的儿童中,分别有27%(22.9%至31.7%)、14%(12.1%至15.9%)和7%(4.4%至9.0%)使用学校援助。在24-26周出生的儿童中,约有一半(52%(46.4%至57.3%))接受了至少一项发育干预,而在32-34周出生的儿童中,这一比例降至26%(21.8%至29.4%)。行为是父母最关心的问题。神经发育障碍的比率随着胎龄的减少而增加,并且在低社会经济地位的家庭中更高。
在这一庞大的当代早产儿队列中,该研究报告了5岁半时的发育情况,包括对教育援助的需求,复杂的发展干预,以及父母对孩子发展的关注。每个胎龄组中严重/中度神经发育障碍的发生率仍然很高。在向父母、卫生人员和教师提供咨询时,以及在为早产儿童设计后续和干预方案时,这一全面视角非常重要。额外的教育援助和复杂的发展资源经常被使用,甚至是对出生中度早产儿或没有或轻度神经发育障碍的儿童。接受学校援助或复杂发展干预的儿童比例可能对教育和卫生组织产生重大影响。不应低估这些儿童群体及其家庭所面临的困难。
识别发育特征以理解导致神经发育障碍的病因途径,从而制定预防或干预策略,是一个重要的研究领域。有限的教育和卫生资源可以集中于风险最大的儿童,根据儿童的风险概况进行后续工作,并为父母提供更好的信息,以避免不必要的焦虑。此外,了解父母对孩子发展的关注为确定适当的干预措施提供了更好的可能性。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMJ#
36
学习了
50
#预防干预#
38
#干预措施#
38
#神经发育#
47
#发育#
26
学习
68
又多了一个参考资料
62
学习学习
58