近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇很有趣的研究文章,这项研究旨在调查青春期口吃与年轻成人2型糖尿病之间的关系。

这项基于人群的全国性研究纳入了1980年至2013年期间服过兵役的2193855名16-20岁青少年。受试者青春期口吃需要被言语病理学家进行诊断。截至2016年12月31日,每个人的糖尿病患病状况则通过与以色列国家糖尿病登记处联系来获取。研究人员使用针对社会经济变量、认知能力、并发症和青少年BMI调整后的回归模型来分析其相关性。
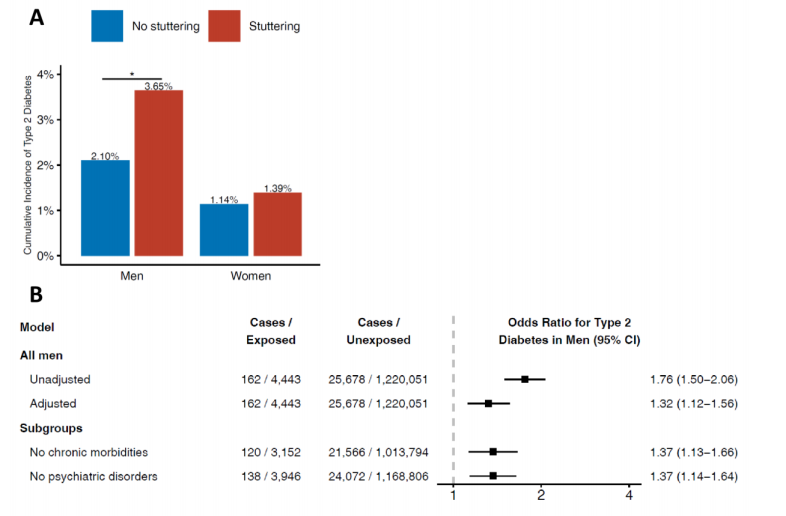
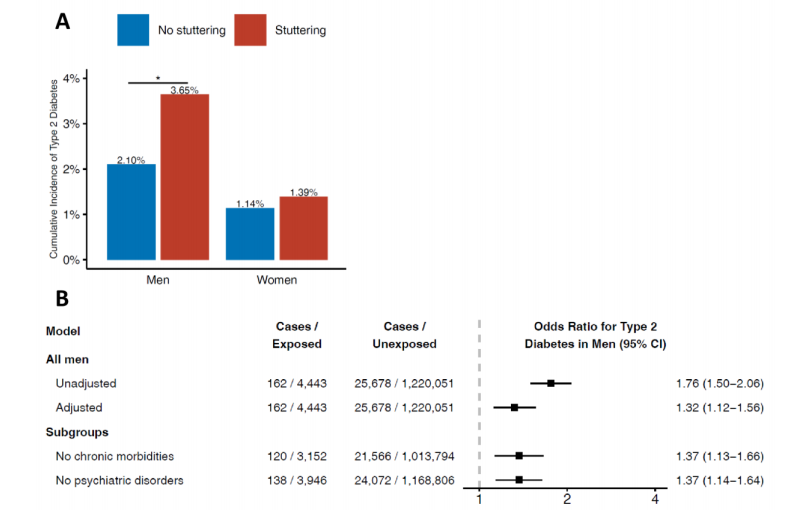
按性别对分析进行了分层(相互作用P=0.035)。在4443名(0.4%)患有口吃的青春期男性中,162名(3.7%)患儿发生2型糖尿病,而没有口吃的男性则为25678名(2.1%)(调整后比值比为1.3,95%CI为1.1–1.6)。当将未患口吃的男性兄弟作为对照组时(调整后的OR=1.5,95%CI为1.01-2.2),或者当分析仅纳入基线时健康状况未受影响的青少年(调整后的OR=1.4,95%CI为1.1-1.7)时,这种关系持续存在。在503例(0.1%)口吃女性中有7例(1.4%)患儿发展为2型糖尿病,相比之下,没有口吃的女性为10139人(1.1%)(OR=2.03,95%CI为0.48-2.20)。
由此可见,青少年口吃与男性罹患早发型2型糖尿病的风险增加相关。
原始出处:
Avishai M Tsur.et al.Stuttering and incident type 2 diabetes: a population-based study of 2.2 million adolescents.JCEM.2021.https://doi.org/10.1210/clinem/dgaa988
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCEM#
33
#口吃#
40
#JCE#
41
啊这……
86
谢谢MedSci提供最新的资讯
60