JAMA:血栓切除成功后加用rtPA能明显改善大血管闭塞急性中风患者功能结局!
2022-02-16 MedSci原创 MedSci原创
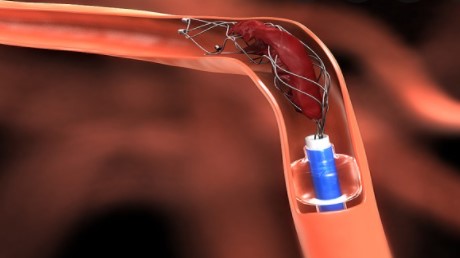
血管内血栓切除术是众多大血管闭塞急性缺血性卒中患者的最佳治疗方案。
血管内血栓切除术是众多大血管闭塞急性缺血性卒中患者的最佳治疗方案。如果在手术结束时,最初受影响的动脉区域有50%至100%以上的再灌注,对应的扩展TICI(eTICI)评分为2b50或更高,则再灌注通常被认为是成功的。
尽管在以前的随机试验中,71%的病人获得了成功的再灌注分数,但只有27%的接受治疗的病人在90天内没有残疾。研究人员猜测有可能在一些患者发生再灌注时,大量的脑组织已经受到不可逆转的损伤。
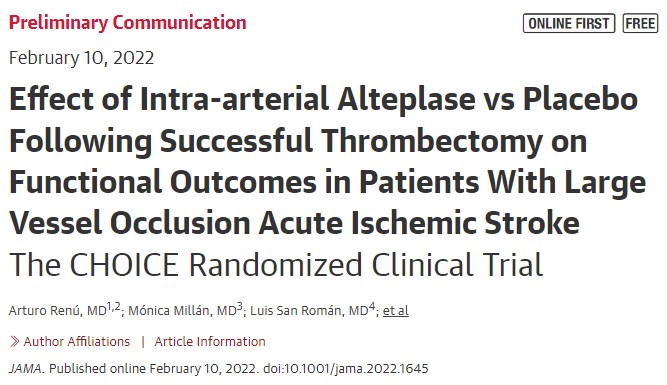
不完全的微循环再灌注可能导致这些不理想的临床效益。为此,来自西班牙巴塞罗那医院综合中风中心神经科学部的专家开展了一项名为CHOICE的临床研究,旨在评估血栓切除术后辅助动脉内rtPA治疗是否能改善再灌注后的结果。结果发表在JAMA杂志上。
这项2b期随机、双盲、安慰剂对照试验于2018年12月至2021年5月在西班牙的7个卒中中心进行,包括121名大血管闭塞且在中风发病后24小时内接受血栓切除术治疗的患者,脑缺血扩大治疗的血管造影评分为2b50-3。参与者随机接受动脉内rtPA 15至30分钟内输注(n = 61)或安慰剂(n = 52)治疗。主要结果是在90天mRS评分0或1分的患者比例的差异。
在7个研究点中,121名(7%)患者被随机分配(平均年龄,70.6[SD,13.7]岁;57名女性[47%]),113名(6%)按随机分配治疗。90天后,阿替普酶的参与者中,mRS评分为0或1的比例为59.0%(36/61),安慰剂为40.4%(21/52)(调整后的风险差异,18.4%;95%CI,0.3%-36.4%;P = 047)。
阿替普酶在24小时内出现症状性颅内出血的患者比例为0%,安慰剂为3.8%(风险差异为-3.8%;95%CI,-13.2%至2.5%)。阿替普酶的90天死亡率为8%,安慰剂为15%(风险差异为-7.2%;95%CI,-19.2%至4.8%)。
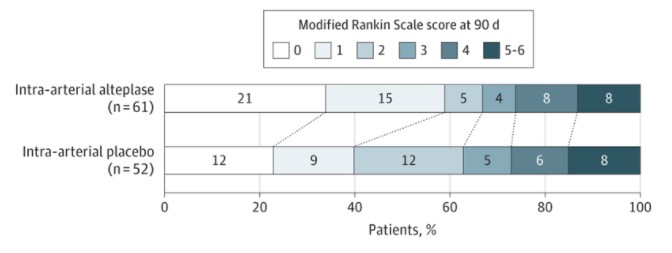
综上,在大血管闭塞急性缺血性卒中患者中,血栓切除术后使用辅助性动脉内阿替普酶,在90天内获得优良神经系统结果的可能性更大。
参考文献:
Effect of Intra-arterial Alteplase vs Placebo Following Successful Thrombectomy on Functional Outcomes in Patients With Large Vessel Occlusion Acute Ischemic Stroke: The CHOICE Randomized Clinical Trial. JAMA. Published online February 10, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#大血管#
50
#血管闭塞#
49
#rtPA#
47
#tPA#
50
#功能结局#
50
#血栓切除#
46
#中风患者#
43