Nature:池洪波/郭傲/黄宏龄等揭示改善实体瘤CAR-T疗效的新方法
2022-06-26 生物世界 生物世界
该研究通过体内 CRISPR 筛选发现了负向调控记忆性 T 细胞形成的关键表观遗传学因子。
CD8+ T 细胞的分化状态与该细胞类群的杀伤功能及其在生理和病理条件下的生存、增殖密切相关。具有干细胞样功能的 T 细胞亚群比如中枢记忆性 T 细胞(central memory T cells,TCM)及记忆性干细胞(T memory stem cells ;TSCM)等已经在病人以及多种小鼠模型中被证实具有更强的抑癌作用。但是,这些亚群的维持机制以及是否可人为控制这些细胞类群的产生还有待进一步研究。
对来自癌症患者免疫细胞进行基因工程修饰的 CAR-T 细胞疗法在血液类癌症中已经显示了强大的疗效,然而,工程化 CAR-T 细胞缺乏持久性这一特点严重阻碍了其对实体瘤的治疗效果。
2022年6月22日,圣裘德儿童研究医院的 Douglas Green 及迟洪波团队合作,在 Nature 期刊发表了题为:cBAF complex components and MYC cooperate early in CD8+ T cell fate 的研究论文。
该研究通过体内 CRISPR 筛选发现了负向调控记忆性 T 细胞形成的关键表观遗传学因子。该研究发现,T 细胞活化早期的 c-MYC 蛋白和 cBAF 蛋白之间的相互作用影响 T 细胞命运,微调这种相互作用可以让幼稚 T 细胞在被肿瘤抗原激活后优先分化为长效记忆性 T 细胞,从而显著提高 CAR-T 细胞治疗实体瘤的效果。

T细胞各亚群均具有不同的表观遗传学谱,因此作者推论表观遗传学因子在T细胞分化和命运决定过程中存在重要作用。作者在前期工作基础上建立了靶向表观遗传学因子的 CRISPR-Cas9 体内筛选系统,并将其用于记忆性 T 细胞的研究中。结果发现,SWI/SNF 染色质重塑复合物亚型 cBAF 的诸多成员是记忆性 T 细胞的负向调节因子。利用多种感染模型,作者揭示了 cBAF 核心成员的缺失促进中枢记忆性 T 细胞的生成、自我更新及二次免疫应答。
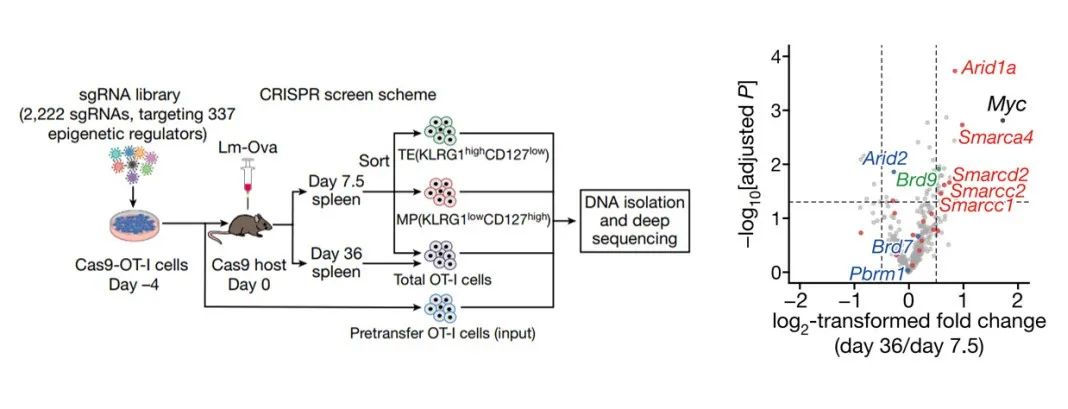
功能基因组学揭示调节SWI/SNF染色质重构复合物亚型cBAF为记忆性T细胞形成的关键负调控机制
T 细胞的不对称分裂对子代细胞向效应 T 细胞及记忆 T 细胞分化有着重要的作用。Douglas Green 课题组近期发表的文章显示,c-Myc 蛋白在不对称分裂过程中在细胞内的定位对这一过程有着重要影响,然而其中的具体机制却并不清楚。
在这项最新研究中,论文作者发现,在 T 细胞的第一次分裂过程中,cBAF 核心成员具有与 c-Myc 类似的细胞内不对称分布。在第一次分裂后的子代细胞中敲除 cBAF 核心组分,能够将子代效应 T 细胞重编程为记忆 T 细胞。紧接着,通过免疫共沉淀、Cut&Run、RNA-seq、ATAC-seq 及遗传学等手段,作者证明 c-Myc 与 cBAF 复合物中多个成员存在相互作用。进一步研究显示,c-Myc 能够促进 cBAF 复合物对相关区域染色质景观的重塑,促进并维持了 T 细胞分化相关基因区域的开放性,从而驱动 T 细胞往效应 T 细胞的方向发育。
Douglas Green 教授表示,如同在生活中一样,早期发生的某些事情决定了事物最终的发展走向;同样,在T细胞激活的早期 c-Myc 与 cBAF 的相互作用最终深刻的影响了 T 细胞的命运。
cBAF 的核心成员参与肿瘤发生等多种生理过程,因此组成型 cBAF 缺失在治疗上可能有潜在的安全隐患。因此,作者试图利用 cBAF 抑制剂在体外短期处理 T 细胞。结果显示,体外短时程的 cBAF 抑制剂处理使得 T 细胞具有记忆性样的转录组并增强 T 细胞在小鼠体内的维持及抗肿瘤能力。最后,cBAF 抑制剂的瞬时处理能提高 CAR-T 的功能及维持力,并能将人外周血单核细胞来源的T细胞重塑至 TSCM 状态。
迟洪波教授表示,这项工作不仅发现 cBAF 复合物是提升 CAT-T 治疗的潜在靶点,而且说明对于免疫系统和 T 细胞功能的深入的理解能够帮助我们开发出更好治疗手段以应对癌症及其它疾病。
总的来说,该研究通过体内 CRISPR 筛选发现了负向调控记忆性 T 细胞形成的关键表观遗传学因子。通过机制分析,发现瞬间的表观遗传学改变即能影响 T 细胞的长效生物学功能,为增强 T 细胞的功能特别是为 CAR-T 细胞的体外培养提供了备选方案。据悉,作者已经申请了相关药物的使用专利。
Douglas Green 课题组郭傲博士及迟洪波课题组黄宏龄博士(现就职厦门大学生命科学学院)为本文的第一作者,Douglas Green 和迟洪波论文的通讯作者。
论文链接:
https://www.nature.com/articles/s41586-022-04849-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CAR-#
50
#实体瘤##CAR-T#疗效的新方法
1
#新方法#
50
#Nat#
46
认真学习了
48
学习了,谢谢分享
46