原发性甲状旁腺功能亢进伴单侧眼球突出
2011-06-09 MedSci原创 MedSci原创
一位27岁女性因双侧肾结石和轻微外伤引起的右侧胫骨骨折来就诊。体格检查:血压124/80 mm Hg,甲状腺I度弥漫性肿大。右眼球突出(23 mm),临床活动度评分为0/7(图 1A),无甲状腺功能亢进的特征。未触及骨肿胀或咖啡牛奶斑。实验室检查:血清钙是3.25 mmol/l (正常为2.15–2.55 mmol/l),无机磷0.77 mmol/l (0.87–1.39 mmol/l
一位27岁女性因双侧肾结石和轻微外伤引起的右侧胫骨骨折来就诊。体格检查:血压124/80 mm Hg,甲状腺I度弥漫性肿大。右眼球突出(23 mm),临床活动度评分为0/7(图 1A),无甲状腺功能亢进的特征。未触及骨肿胀或咖啡牛奶斑。实验室检查:血清钙是3.25 mmol/l (正常为2.15–2.55 mmol/l),无机磷0.77 mmol/l (0.87–1.39 mmol/l),血清甲状旁腺激素(iPTH) 1295 ng/l (15–65 ng/l),血清碱性磷酸酶66.1 μmol/l (0.67–2.02 μmol/l),提示原发性甲状旁腺功能亢进。
甲状腺功能检查:T3 (三碘甲状腺原氨酸) 2.26 nmol/l,T4 (甲状腺素) 71.75 nmol/l, TSH (促甲状腺激素) 3.84 mU/l,抗甲状腺过氧化物酶抗体(6.36 U/l) 均是正常的。颈部超声和锝99m MIBI(甲氧基异丁基异睛)扫描发现左上甲状腺旁有一个腺瘤。CT平扫显示右侧眼眶有一处溶解性膨胀性病灶,提示为囊性纤维性骨炎(OFC),但眼眶肌是正常的(图1B)。患者做了普通根治性甲状旁腺切除术。3个月后,眼球突出有所消退(23mm 缩小为 21 mm) (图2A),CT扫描显示骨溶解性病灶已愈合(图2B)。
图1 (A)临床图片示右眼球突出。(B)眼眶CT扫描显示囊性纤维性骨炎。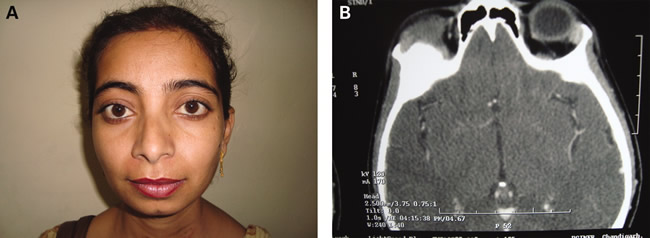
(A)术后临床图片示突眼改善。(B)术后眼眶CT扫描示骨溶解性病灶已愈合。
囊性纤维性骨炎常见于皮质骨和扁平骨,是甲状旁腺激素(PTH)过量的表现。累及眼眶骨的报告罕见[1-2] 。目前已有关于额骨和泪骨囊性纤维性骨炎的报告,表现为单侧眼球突出。其中一个病例进行了细针穿刺细胞学(FNAC) 检查,确诊为囊性纤维性骨炎。然而,此项操作只能应用于易进入的病灶。本病例未行此项检查,但是根治性甲状旁腺切除术后患者突眼程度减轻且CT显示病灶愈合证实了囊性纤维性骨炎与本病相关。
参考文献
[1] Fatourechi V, Bastanhagh MH. Primary hyperparathyroidism presenting as unilateral exophthalmos. Acta Medica Iranica 1996: 29–32.
[2] Naiman J, Green WR, dHeurle D, et al. Brown tumor of the orbit associated with primary hyperparathroidism. Am J Opthalm 1980: 565–71.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#原发性#
32
#眼球#
42
#甲状旁腺功能亢进#
29
#甲状旁腺#
38
#原发性甲状旁腺功能亢进#
35