EHJCP:塞来昔布与萘普生或布洛芬治疗关节炎的心肾风险比较
2022-03-23 医路坦克 MedSci原创
非甾体抗炎药是全世界最常用的止痛药,在关节炎患者中的长期心血管安全性引起了争议,本文旨在进一步在PRECISH试验中测试的三种非类固醇抗炎药的心肾安全性。
非甾体抗炎药是全世界最常用的止痛药,每天有3000多万人服用,其中许多人患有骨关节炎。面对人口老龄化和阿片类药物过度使用的流行,疼痛管理,特别是关节炎引起的疼痛管理,已经变得越来越紧迫。第一代NSAIDs非选择性抑制环氧合酶(COX),如消炎痛、萘普生和布洛芬。与这些药物相关的胃肠道不良反应(溃疡、出血、穿孔)刺激了选择性COX-2抑制剂的开发,如罗非昔布和塞来昔布。自2004年罗非昔布退出市场以来,塞来昔布仍然是目前美国唯一可用的选择性抑制剂。对选择性COX-2抑制剂安全性的大部分担忧源于它们缺乏抗血小板活性,以及失去潜在的血管扩张剂和非选择性COX抑制的抗增殖特性,这些特性可能促进血栓的形成。此外,由于肾组织结构性地表达COX-2,许多医生避免在肾功能减退的患者中使用所有非甾体抗炎药。来自CLASS7和Vigor试验3以及多个子分析和专案研究的相互矛盾的结果促使人们对选择性COX-2抑制剂的心血管安全性进一步持保留意见。事实上,许多骨关节炎和类风湿性关节炎患者也有心血管危险因素或已确定的冠状动脉疾病。因此,FDA就使用这类药物引发心脏病发作和中风的风险发出了多次警告。
PRECISE试验解决了三种研究药物中有关心血管相对安全性的问题。PRECISE试验显示,在所研究的剂量下,塞来昔布并不比萘普生和布洛芬差,在数字上塞来昔布组的心血管事件数量较少。精密度的初步分析显示,总体上表明塞来昔布的肾脏安全性更有利,这一初步发现需要更详细的分析。因此,目前的二次分析旨在进一步在PRECISH试验中测试的三种非类固醇抗炎药的心肾安全性。
24,081名因骨关节炎或类风湿关节炎而需要非类固醇抗炎药且心血管风险增加的患者随机接受塞来昔布、布洛芬或萘普生治疗。目前的预先指定的二次分析评估了意向治疗(ITT)人群中预先指定的综合心肾结果[已判定的肾事件、因充血性心力衰竭(CHF)住院或因高血压(HTN)住院]的发生率、严重性和非甾体抗炎药相关风险。一项治疗分析评估了那些服用研究药物的人的安全性。
在平均治疗时间20.3、16.0个月和平均随访34.1月、13.4个月后,423名患者(1.76%)出现了原发心肾综合结局。在这423例患者中,塞来昔布组118例(28%),布洛芬组166例(39%),萘普生组139例(33%)。在调整了独立临床变量的多变量COX回归模型中,塞来昔布与布洛芬相比风险显著降低(风险比0.67,可信区间0.53-0.85,p=0.001),与萘普生相比有降低风险的趋势(风险比0.79,可信区间0.61-1.00,p=0.058)。在意向治疗分析中,220例患者发生了临床显著的肾脏事件,事件发生率分别为0.71%、1.14%和0.89%(p=0.052)。而在治疗分析中,有效率分别为0.52%、0.91%和0.78%(P<0.001)。
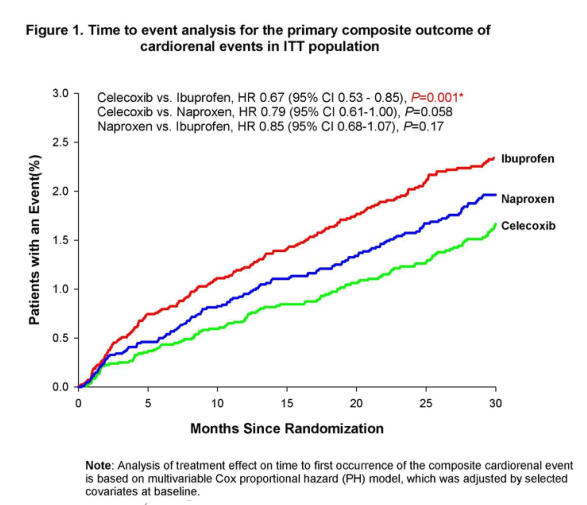

结论:长期使用非甾体类抗炎药与关节炎患者心肾不良反应发生率较低。在所研究的剂量下,与布洛芬或萘普生相比,塞来昔布表现出较少的肾脏事件,因此对心血管安全更有利。这些结果对于管理患有慢性关节炎疼痛和肾功能受损和/或心力衰竭高风险的个体的从业者具有相当大的临床意义。
文献来源:Obeid S, Libby P, Husni E, Cardiorenal Risk of Celecoxib compared to Naproxen, or Ibuprofen in Arthritis Patients: Insights from the PRECISION trial.Eur Heart J Cardiovasc Pharmacother 2022 Mar 02;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#风险比#
47
#关节炎#
46
#塞来昔布#
68
#萘普生#
53