中国超过5万名儿童研究,布洛芬可显著增加急性肾损伤风险!
2021-03-05 MedSci原创 MedSci原创
布洛芬是一种非甾体类抗炎药(NSAID),是一种非选择性的环氧合酶阻滞剂。
布洛芬是一种非甾体类抗炎药(NSAID),是一种非选择性的环氧合酶阻滞剂。在美国,估计每天有3600万人使用非处方镇痛药,并且每年分发的非处方药NSAID处方超过1.11亿。目前,在美国,每年布洛芬的处方药超过2000万份。作为环氧合酶活性的阻滞剂,布洛芬用于儿童烧,术后疼痛,肿瘤和炎性疾病,然而,有研究显示,成人和儿童使用非甾体抗炎药物可能会增加急性肾损伤(AKI)的风险。尽管布洛芬是世界上最常用的非甾体抗炎药,但很少有大型研究专门研究布洛芬与儿童AKI发病率之间的关联。

近日,发表在JAMA Netw Open杂志上的一项研究显示,在中国住院儿童中,布洛芬被广泛使用,并与AKI风险增加有关。在使用布洛芬时,需慎重并密切监测儿童的肾功能。这是中国首个儿童布洛芬使用与医院获得性AKI的大型队列研究。
该队列研究分析了中国住院患者AKI流行病学(EACH)研究的队列,共有3044023名年龄在1个月至18岁之间的住院患者,其中包含50420名儿童,平均年龄为5岁,60.8%为男孩。研究人员从参与中心的电子健康记录系统获得了患者健康数据,包括年龄,性别,诊断日期,出院时的诊断代码,手术程序和日期,重症监护需要,院内死亡以及总住院费用。实验室数据包括血清肌酐(SCr)测试的结果和时间。处方数据包括处方药或程序的名称,剂量以及开始和停止时间。通过Cox比例风险回归模型探索布洛芬的使用与医院获得性AKI风险之间的相关性。
结果显示,有5526名(11.0%)使用布洛芬,3476名(6.9%)发展为医院获得性AKI。在调整混杂因素后,布洛芬的使用可增加医院获得性AKI发病风险(危险比[HR],1.23;95% CI,1.14-1.34)。与患有慢性肾脏疾病的儿童相比,使用布洛芬的儿童患AKI患病风险更大(HR:2.31 [95%CI,1.73-3.10] vs 1.19 [95%CI,1.09-1.29]),尤其是年龄较大或需要重症监护的儿童(>10岁和>1年至10岁 vs 1个月至1年)(HR,1.64 [95% CI,1.32-2.05];1.36 [95% CI,1.23-1.52] vs 0.99 [95% CI,0.86-1.13])。在剂量反应分析中,布洛芬的使用剂量与医院获得性AKI风险呈正相关。
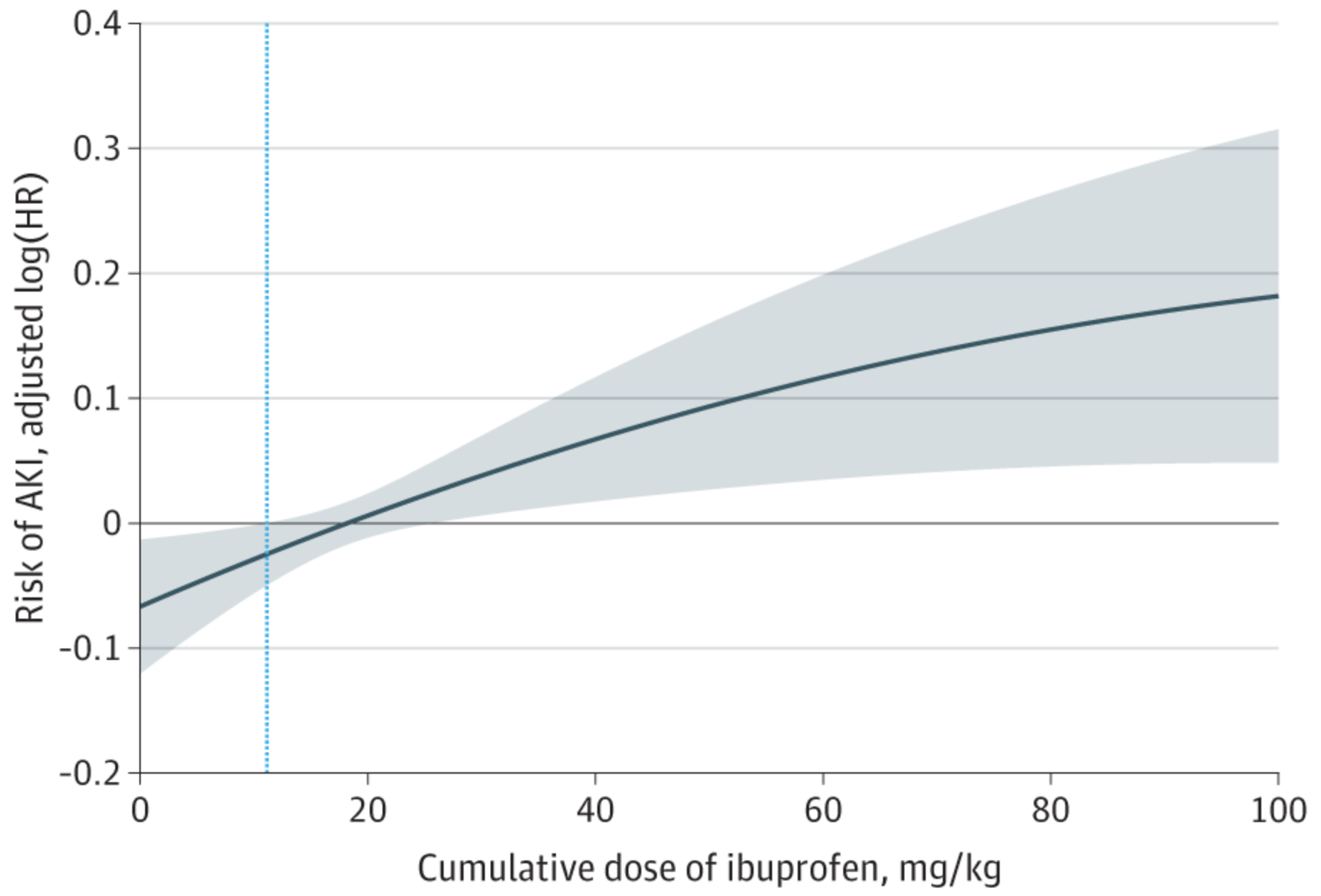
医院获得性急性肾损伤(AKI)风险和布洛芬累积剂量的剂量反应曲线

总之,这项大型,多中心,回顾性队列研究表明,中国住院儿童中普遍使用布洛芬,并且在调整混杂因素后,医院获得性AKI的风险显著增加,而且与剂量呈现依赖性关系。
原始出处
Licong Su, MD1; Yanqin Li, MD1; Ruqi Xu, MD1; et al.Association of Ibuprofen Prescription With Acute Kidney Injury Among Hospitalized Children in China.JAMA Netw Open. 2021;4(3):e210775. doi:10.1001/jamanetworkopen.2021.0775
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#损伤#
52
学习了!!
111
学习了
111
学习了
122
学习了
111