Med Image Anal:国际领先!中山六院实现人工智能结肠癌病灶影像精准分割
2022-07-13 中山六院 中山六院
当前,能否实现全自动的、精准的病灶分割是决定医学影像在临床使用效果的关键。
CT作为一种常见的检查手段,相信不少老百姓均十分熟悉。而基于影像的自动分割技术能够辅助医生精确了解病灶的位置、大小以及与周围血管、组织的关系,帮助疾病诊断、图像引导手术以及医学数据的可视化,为临床诊疗和病理学研究提供可靠的依据。
当前,能否实现全自动的、精准的病灶分割是决定医学影像在临床使用效果的关键。
近年来,深度神经网络的快速发展使得许多先进的分割方法都取得了可喜的进展。但与肝脏、心脏等器官相比,肠道肿瘤的形态、位置的变化大,因此,肠道肿瘤的自动分割任务难度高。特别是结肠癌,因病灶分布范围大、解剖结构复杂,一直未能实现有效的病灶自动分割,这一现状严重制约了肠癌精准诊疗人工智能的临床应用。

▲Medical Image Analysis发表吴小剑教授团队牵头完成的研究成果
近日,我院结直肠肛门外科吴小剑团队迈出了坚实的一步。他们在国际上率先实现了自主结肠癌病灶影像精准分割的人工智能临床解决方案,源于其开发的结肠癌病灶自动精准分割的医学影像人工智能弱监督-半监督框架(Segmentation Only Uses Sparse Annotations,SOUSA )。
相关研究结果在医学影像人工智能算法顶刊Medical Image Analysis(IF=13.828)发表。
本研究由吴小剑教授团队牵头,联合喀什地区第一人民医院邹小广教授团队、上海人工智能实验室协作完成。
其中,文章题为“Segmentation only uses sparse annotations: Unified weakly and semi-supervised learning in medical images”(只使用稀疏标注的病灶分割:医学图像的联合弱学习和半监督学习),吴小剑教授为最后通讯作者,喀地一院邹小广教授、上海交通大学张晓凡教授为共同通讯作者,我院高峰副研究员、钟敏儿博士、孟晓春主任与喀地一院田序伟主任为共同第一作者,喀地一院马依迪丽·尼加提主任等为共同作者。
据介绍,基于医学影像的人工智能为肠癌个体化诊疗提供了巨大的可能性,已经有多项研究实现了病人的疗效预测、术后复发风险评估,但这些应用无不依赖于精准的病灶分割。
此次SOUSA技术的开发在国际上首次实现了结肠癌的自动分割,为加速肠癌人工智能精准诊疗的临床应用奠定了基础。
自动化标准化的精准影像信息处理将有效地降低经济、时间和人力成本,为精准诊疗的实施提供了重要的临床依据,具备极大的临床转化应用前景。
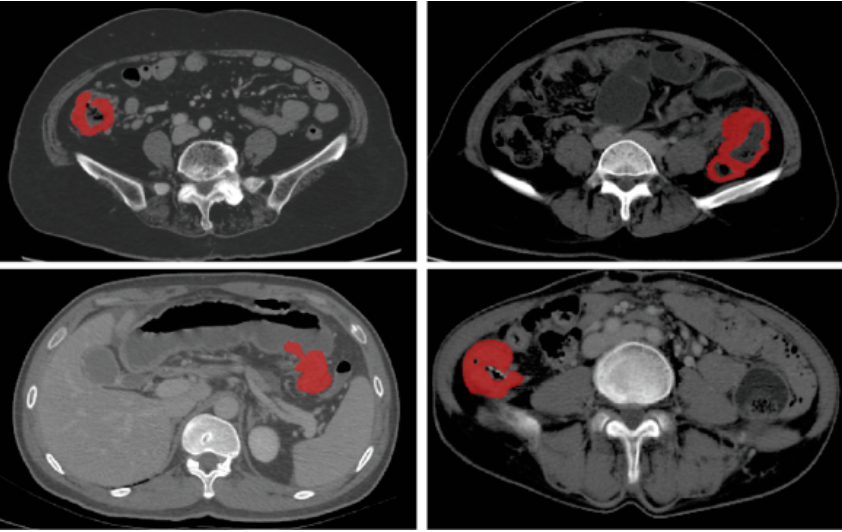
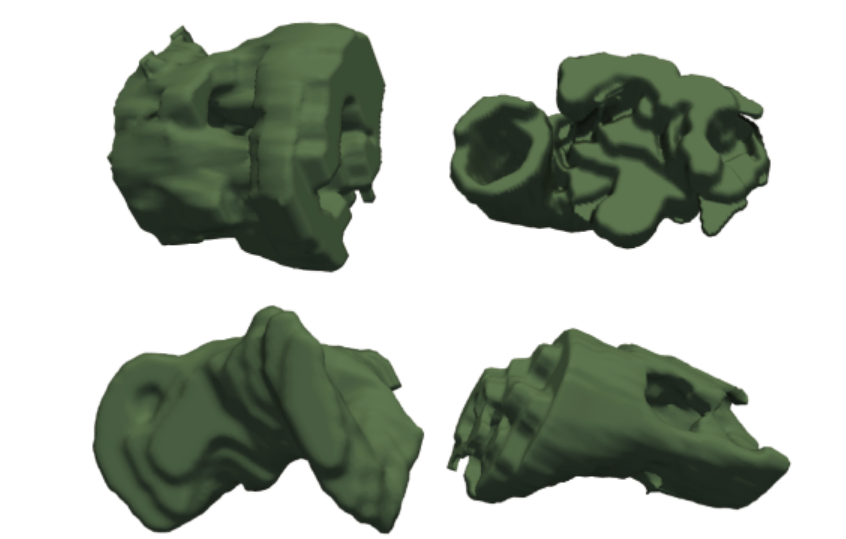
▲基于CT影像的结肠癌病灶分割
本研究中,团队在SOUSA框架中充分利用了弱监督学习和半监督学习的优势,提高了人工智能的学习效率,减少了假阳性的预测,显著提高了病灶分割的准确度。
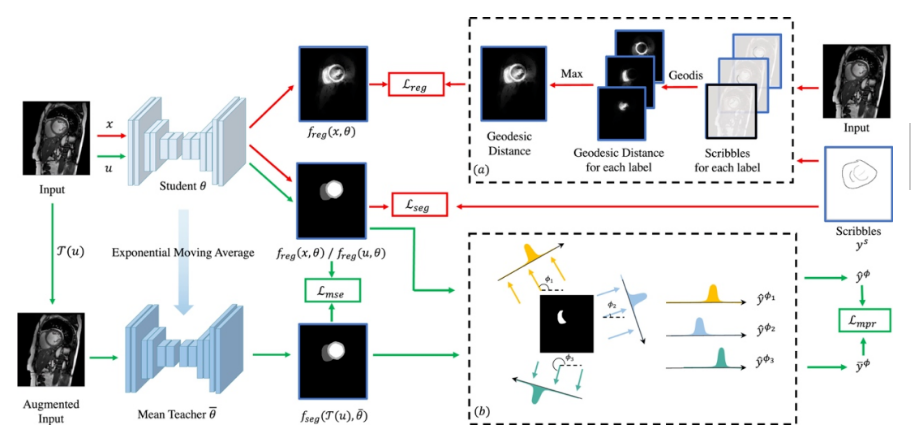
▲SOUSA框架
团队利用来自中山六院和喀地一院的923例有标注结肠癌CT影像和2670例无标注结肠癌CT影像作为SOUSA框架的训练数据集,并利用417例结肠癌CT影像对SOUSA框架进行验证,结果显示其自动分割效果优于现有的弱监督和半监督学习模型。与目前最先进的方法ICT (Verma et al.,2019)、不确定性感知(Yu et al.,2019)和自我训练相比,SOUSA框架在每个数据比率上都达到了最佳性能。此外,当数据集的大小有限时,SOUSA框架的性能甚至与使用密集注释的模型的性能相当。
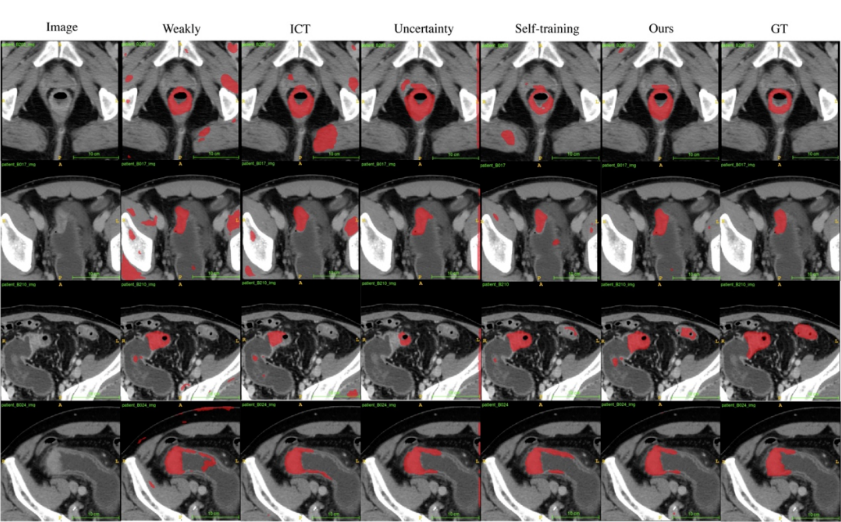
▲对肠癌数据集使用不同方法的自动分割结果
受中山大学选派,自去年6月27日起,现任广东省援疆医疗队队长、喀地一院院长、我院副院长吴小剑投身为期一年半的援疆工作。
援疆期间,吴小剑立足当地学科建设,发挥该院团队特长,以SOUSA框架这一粤喀合作成果切实助力喀地一院发展。
原文链接:
Feng Gao, et al. Segmentation Only Uses Sparse Annotations: Unified Weakly and Semi-Supervised Learning in Medical Images. Medical Image Analysis. Available online 17 June 2022.
https://doi.org/10.1016/j.media.2022.102515
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ANA#
44
#Anal#
64
#精准#
54
#Med#
46