J Clin Oncol:Avapritinib对比瑞戈非尼(Regorafenib)治疗局部进展不可切除或转移性胃肠道间质瘤的疗效:随机III期研究
2021-08-04 yd2015 MedSci原创
avapritinib对比瑞戈非尼(Regorafenib)三线或以上治疗局部进展不可切除或转移性胃肠道间质瘤的PFS没有统计学差异。
KIT 或PDGFRA的原发或继发性突变可导致大部分胃肠道间质瘤(GIST)患者对TKI的耐药。Avapritinib 可选择的有力抑制KIT和PDGFRA。在I期研究NAVIGATOR (NCT02508532)中,avapritinib对伴有PDGFRA D842V突变和KIT突变GIST展示出临床活性。因此,研究者开展III期研究VOYAGER (NCT03465722), 评估Avapritinib对比瑞戈非尼(Regorafenib)三线或以上治疗局部进展不可切除或转移性胃肠道间质瘤的疗效和安全性。相关结果发表在Journal of Clinical Oncology杂志上。

患者随机1:1分配至avapritinib 300 mg/每天或瑞戈非尼160mg/每天(服用3周休息1周)。主要研究终点为PFS。次要研究终点为ORR、OS、DCR、DoR和安全性。瑞戈非尼治疗进展后可交叉至avapritinib治疗。
研究纳入476例患者,其中avapritinib治疗有240例,瑞戈非尼有236例。有41.9% (99 of 236) 患者交叉至avapritinib 治疗。意向性人群中,中位年龄为61 (31-91)岁,66.8% (318 of 476)为男性, 59.2% (282 of476) 为白种人, 25.4% (121 of 476)为亚洲人群。所有患者既往接受过伊马替尼,95.0% (452 of 476) 患者既往接受过sunitinib。基线检测时,PDGFRA 18外显子突变为3.8% (18 of 476),2.7% (13 of 476) 有PDGFRA 18外显子D842V 突变。
Avapritinib 和 regorafenib治疗的中位PFS没有明显差异,分别为4.2和5.6个月(HR=1.25; 95% CI, 0.99 to 1.57; P=0 .055)。类似的,两组作为三线治疗的中位PFS没有统计学差异(HR=1.26;95% CI, 0.98 to 1.61; mPFS 4.2 v5.5个月;P=0.068) 或四线治疗也没有统计学差异(HR=1.19; 95%CI, 0.66 to 2.15; mPFS 3.8 v 5.6个月;P=0.550)。PDGFRA D842V突变患者(n=13), avapritinib 治疗的mPFS (not reached [NR]; 95% CI, 9.7 to NR)较瑞戈非尼(4.5个月; 95% CI, 1.7 to NR; P =0.035)明显延长。排除PDGFRA D842V突变患者,其他患者中,瑞戈非尼治疗较avapritinib明显延长mPFS(HR, 1.34; 95% CI, 1.06 to 1.69; mPFS 3.9 v 5.6个月;P=0.012)。
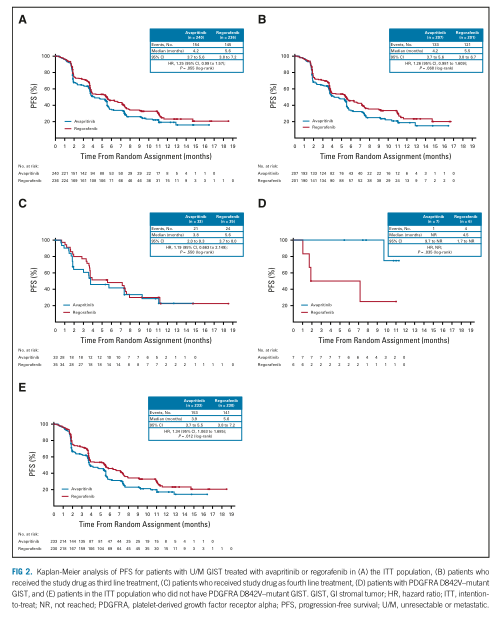
PFS
数据截止时,两组的中位OS尚不成熟。12个月评估的OS率分别为68.2%和67.4%。三线治疗时分别为67.9%和68.8%;而作为四线治疗时分别为67.4% 和60.4%。avapritinib 组(17.1%; 95% CI, 12.5 to 22.5; all PR)的ORR较瑞戈非尼(7.2%; 95% CI, 4.3 to 11.3; all PR)明显增高(P<0.001)。两组的DOR分别为7.6个月(95%CI,5.6 to NR) 和 9.4个月(95% CI, 7.4 to NR)。两组的疾病控制率(DCR) 分别为41.7% (95%CI,35.4to48.2)和46.2% (95%CI,39.7to52.8)。

疗效评估
任何级别治疗相关不良事件(TRAEs)中,两组分别为92.5%和96.2%。≥3 级TRAEs的比例分别为55.2%和57.7%。avapritinib 治疗常见的不良反应为贫血(40.2%), 恶心(39.3%), 和疲劳 (35.1%);而瑞戈非尼常见的为疲劳(34.2%),腹泻(34.6%),和手足综合征(59.0%)。
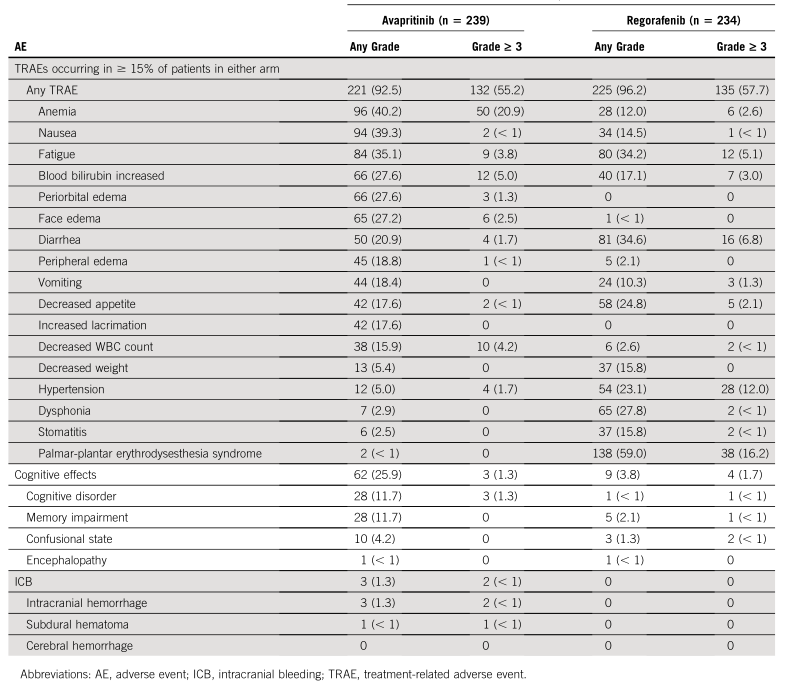
不良事件
综上,avapritinib对比瑞戈非尼(Regorafenib)三线或以上治疗局部进展不可切除或转移性胃肠道间质瘤的PFS没有统计学差异。
原始出处:
Kang YK, George S, Jones RL, et al. Avapritinib Versus Regorafenib in Locally Advanced Unresectable or Metastatic GI Stromal Tumor: A Randomized, Open-Label Phase III Study. J Clin Oncol. 2021 Aug 3:JCO2100217. doi: 10.1200/JCO.21.00217. Epub ahead of print. PMID: 34343033.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#APRI#
30
#Oncol#
26
#III期研究#
37
#Avapritinib#
38
#VAP#
44
#III#
22
#胃肠道#
46
#转移性#
27
#局部#
23
#间质瘤#
0