Lancet Gas Hepa:患者呼吸道样本检测转阴后,其粪便样本仍可呈阳性近5周!
2020-04-02 医学论坛网 医学论坛网
近日,珠海市中山大学附属第五医院感染与免疫研究中心主任黄曦教授团队,在国际顶级医学期刊《柳叶刀胃肠病学和肝病学》在线发表了一篇关于粪便样品中新冠病毒RNA的存在时间的研究文章。
先前,钟南山、李兰娟院士团队近日分别从新冠肺炎患者的粪便样本中分离出新型冠状病毒。而粪便中存在病毒或其他病原,是发生粪口传播的必要条件,但并不意味着疾病一定能通过“粪-口”即消化道途径传播。病毒通过粪便甚至是尿液排泄,是病毒入血后长时间待在血里可能存在的表现;尤其当病毒血症持续的时间越长,粪便或尿液能够排泄病原的时间可能就越长。
近日,珠海市中山大学附属第五医院感染与免疫研究中心主任黄曦教授团队,在国际顶级医学期刊《柳叶刀胃肠病学和肝病学》在线发表了一篇关于粪便样品中新冠病毒RNA的存在时间的研究文章。
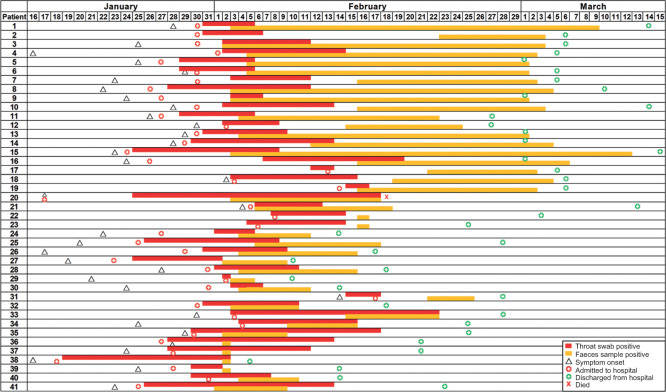
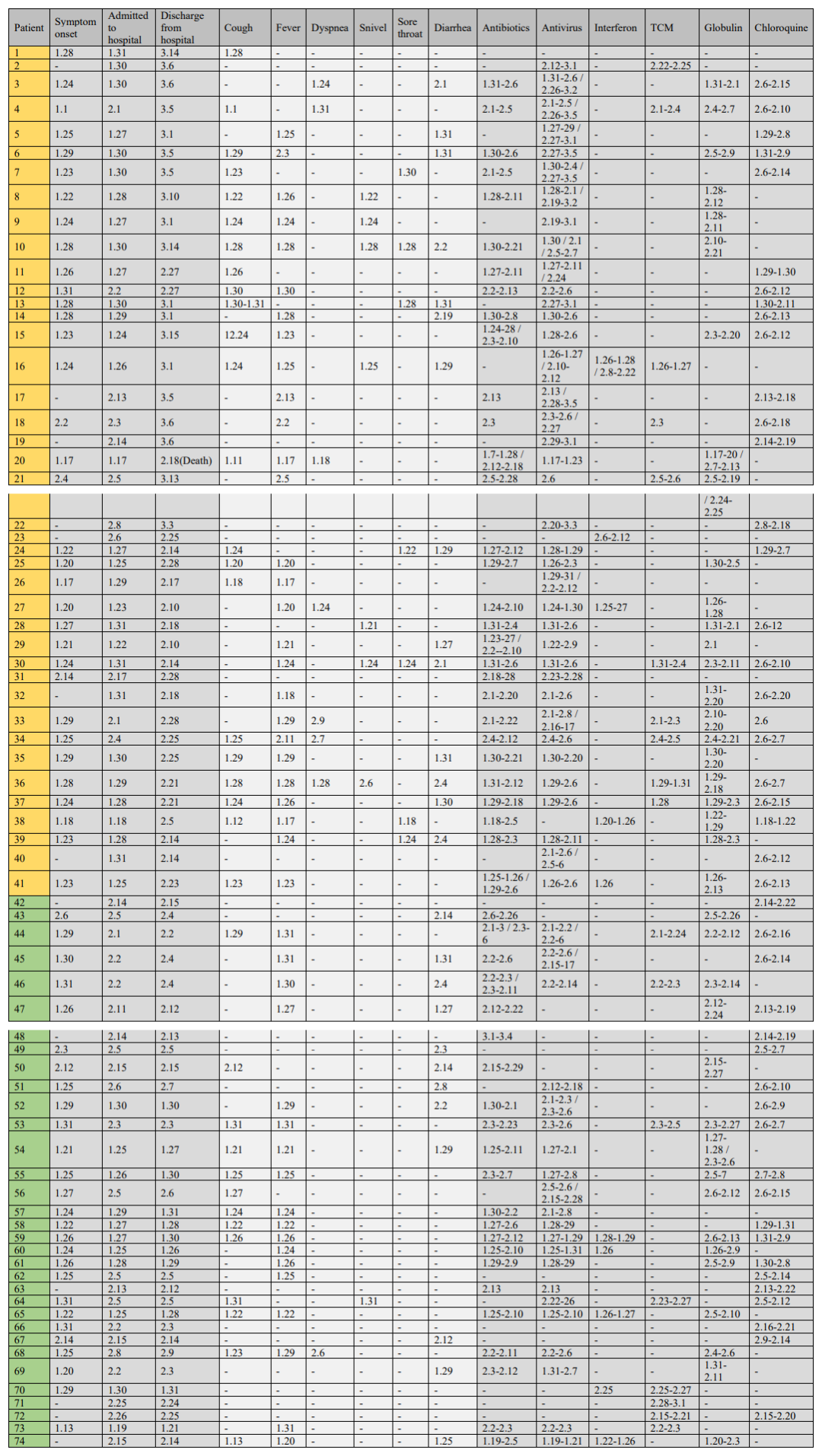
文章报告了珠海市中山大学第五附属医院新冠肺炎患者在整个病程和强制检疫期内呼吸道和粪便标本的新冠病毒实时RT-PCR结果。疑似新冠肺炎的患者在连续两次呼吸道样本呈阳性得到确诊后,每1-2天收集一次呼吸道和粪便样本(取决于粪便样本的可用性),直到获得两个连续的阴性结果。研究回顾了患者的人口统计信息,潜在疾病,临床指标,以及他们的官方医疗记录中的治疗。
研究从2020年1月16日到3月15日,共登记了98名患者。从74例(76%)患者中采集了呼吸和粪便样本。74名患者中有33名(45%)的粪便样本中新冠病毒RNA阴性,而他们的呼吸拭子自首次出现症状以来平均保持阳性15.4天(SD 6.7)。41例(55%)新冠病毒RNA阳性的粪便标本中呼吸道标本平均16.7天(SD 6.7)保持新冠病毒RNA阳性,粪便标本在首次症状发作后平均27.9天(10.7)保持阳性,平均11.2天[9.2]比呼吸样本长)。值得注意的是,患者1在呼吸道样本呈阴性后连续33天粪便样本呈阳性,患者4在首次症状发作后47天粪便样本中检测到新冠病毒RNA呈阳性。
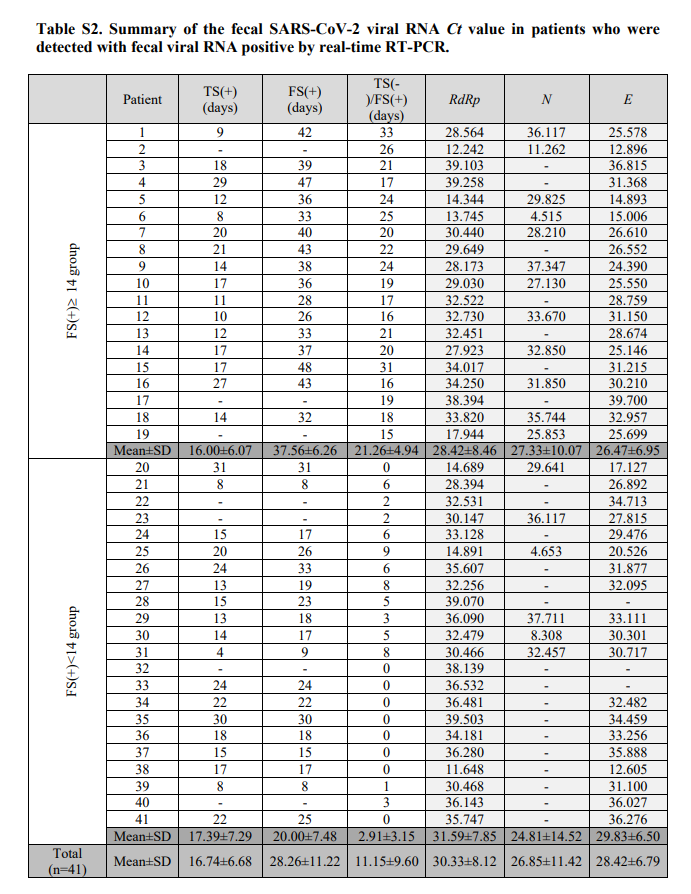 胃肠道症状的出现与粪便样本病毒RNA阳性无关(p=0.45);疾病的严重程度与粪便样本病毒RNA阳性持续时间无关(p=0.60);而抗病毒治疗与粪便样本病毒RNA阳性存在正相关(p=0.025)。在第一个粪便样本中,病毒RNA阳性的三个靶基因(RdRp,N,E)的Ct值与粪便病毒RNA阳性持续时间呈负相关(RdRp基因r=-0.34;N基因r=-0.02;E基因r=-0.16),而Ct值与粪便样本阳性持续时间呈负相关仅对RdRp有显著意义(p=0.033;N基因p=0.91;E基因p=0.33)。
胃肠道症状的出现与粪便样本病毒RNA阳性无关(p=0.45);疾病的严重程度与粪便样本病毒RNA阳性持续时间无关(p=0.60);而抗病毒治疗与粪便样本病毒RNA阳性存在正相关(p=0.025)。在第一个粪便样本中,病毒RNA阳性的三个靶基因(RdRp,N,E)的Ct值与粪便病毒RNA阳性持续时间呈负相关(RdRp基因r=-0.34;N基因r=-0.02;E基因r=-0.16),而Ct值与粪便样本阳性持续时间呈负相关仅对RdRp有显著意义(p=0.033;N基因p=0.91;E基因p=0.33)。
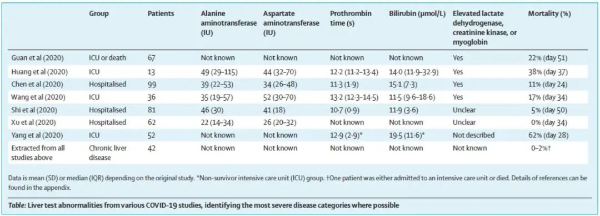
研究数据表明,在患者的呼吸道样本检测出新冠病毒RNA呈阴性后近5周内,粪便中仍可检测到新冠病毒 RNA。该病毒可能在环境中存活数天,这可能导致粪-口传播。因此,强烈建议在清除患者呼吸道样本中的病毒RNA后,使用实时RT-PCR进行常规粪便样本测试。如果住院或自我隔离的粪便样本检测呈阳性,则应采取严格的预防措施以防止传播。粪便样本中新冠病毒RNA的阳性率通常落后于呼吸道样本,因此不建议在现有的新冠肺炎诊断程序中增加粪便样本的检测,决定何时停止预防措施以防止从新冠肺炎恢复的患者中传播,对于医疗资源的管理至关重要。还没有通过粪便-口腔途径传播新冠病毒的病例报告,这可能意味着在隔离设施、医院或在自我隔离的情况下,不太可能通过这条途径感染。然而,潜在的粪便-口腔传播可能会增加旅馆、宿舍、火车、公共汽车和游轮等场所的传播风险。
新冠病毒通过粪便和口腔传播的可能性有一定的影响,特别是在卫生条件差的地区。冠状病毒易受含乙醇的防腐剂和含氯或漂白剂的消毒剂的影响,在处理冠状病毒感染患者的粪便时必须严格遵守预防措施,医院污水也应适当消毒。应强调经常和适当的手卫生的重要性。
原始出处:
Yongjian Wu, Cheng Guo, Lantian Tang, et.al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. The Lancet Gastroenterology and Hepatology March 19, 2020
Charleen Yeo, Sanghvi Kausha, Danson Yeo. Enteric involvement of coronaviruses: is faecal–oral transmission ofSARS-CoV-2 possible? The Lancet Gastroenterology and Hepatology February 19, 2020
Michelle L. Holshue, Chas DeBolt, Scott Lindquist, et.al. First Case of 2019 Novel Coronavirus in the United States. NEJM March 5, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#样本#
25
#GAS#
27
#Lancet#
30
#呼吸道#
26
#EPA#
19
#粪便#
39
临床意义何在?
63