Eur Radiol:如何使用放射组学提高预测胶质母细胞瘤患者生存期?
2021-02-25 shaosai MedSci原创
放射组学通过将影像学图像转化为大量标准化的特征,克服了人眼的主观因素影响,从而实现了对影像学图像的定量分析。
胶质母细胞瘤是最常见的原发恶性脑肿瘤,预后较差。在目前标准的手术切除治疗下,中位生存期约为14个月。一小部分存活时间超过3年的患者被认定为长期存活者。因此,确定影响患者长期生存的预后因素是临床极为关注的方面,这反过来也为患者的早期风险评估提供了依据。
目前确定的胶质母细胞瘤预后因素包括临床因素,如年龄、手术切除方式,以及遗传因素,如异柠檬酸脱氢酶-1 (IDH1)突变状态和O-6甲基鸟嘌呤- dna -甲基转移酶(MGMT)启动子甲基化状态。一些常规的MR影像表现,如术前肿瘤体积、瘤周水肿程度、增强程度和坏死程度,也被发现与胶质母细胞瘤的预后相关。
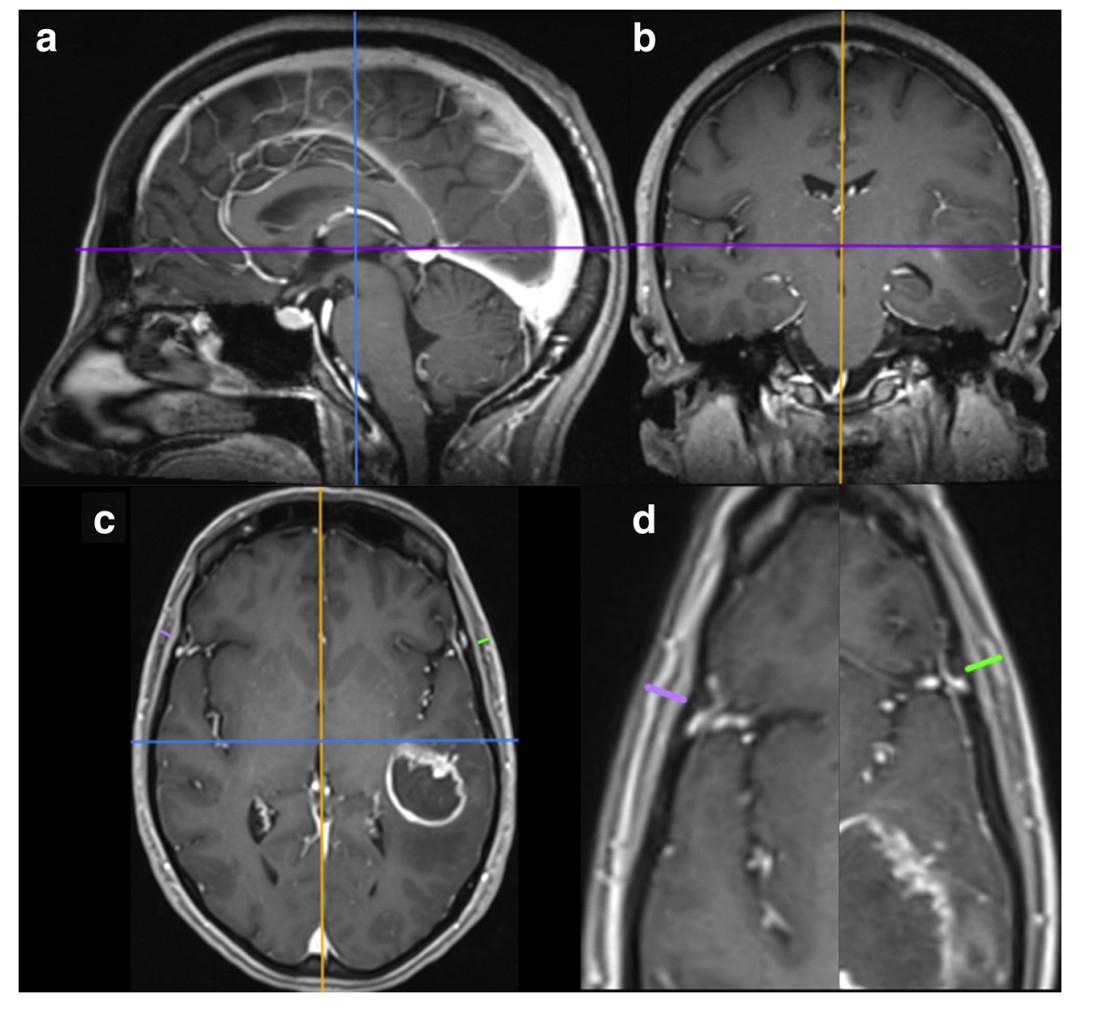
近几年,胶质母细胞瘤患者治疗前的放射组学的风险分层越来越被人们所关注。放射组学通过将影像学图像转化为大量标准化的特征,克服了人眼的主观因素影响,从而实现了对影像学图像的定量分析。目前较多研究发信,建立在传统临床和遗传模型结合的放射组学预后模型在预测生存期方面效果最佳。而在进行放射组学分析前,首先需要在MRI图像上对胶质母细胞瘤进行分割。然而,在多参数MR图像中,手工分割胶质母细胞瘤的子区域是一个非常耗时的过程,且容易出现不同评分者之间的差异。为了克服这一障碍,最近的一些研究使用了基于卷积神经网络(CNN)的算法对胶质母细胞瘤图像进行全自动分割。
近日,发表在European Radiology杂志的一项研究表明使用基于CNN的亚区域分割和各种预后因素生存预测的整合将有助于对胶质母细胞瘤患者进行有效和早期的风险评估。
在本项单中心研究中,对2007年10月至2019年12月间诊断为胶质母细胞瘤的患者进行回顾性的筛查,并按7:3的比例将其分组为训练集和测试集。使用多参数MRI通过卷积神经网络自动完成胶质母细胞瘤的分割。临床模型中的预后因素包括年龄、性别、术式/术后治疗方式和肿瘤位置;遗传模型包括异柠檬酸脱氢酶-1突变和O-6-甲基鸟嘌呤-DNA-甲基转移酶启动子甲基化的状态。对总生存期(OS)和无进展生存期(PFS)进行了单因素和多因素Cox比例风险分析。通过bootstrapping方法计算生存率曲线下积分时间依赖性面积(iAUC),并在预后模型之间进行比较(通过预测误差曲线验证性能)。
本研究共纳入120例患者(训练组85例,测试组,35)。平均OS和PFS分别为25.5个月和18.6个月。当放射组学结合临床模型(iAUC: OS, 0.62 - 0.73;PFS, 0.58 ~ 0.66)、结合遗传模型(iAUC: OS, 0.59 ~ 0.67;PFS, 0.59 ~ 0.65)以及组合模型(iAUC: OS, 0.65 ~ 0.73;PFS, 0.62至0.67)时,多变量模型的预后性能得到明显提高。在试验集中,组合模型(临床、遗传和放射组学)证明了对OS和PFS的风险预测的可靠验证。
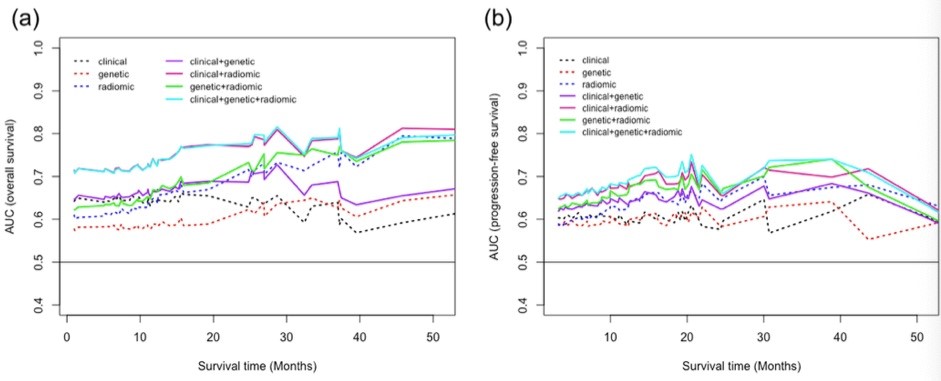
图1 (a)总体生存率(b)无进展生存期的iAUC。如图所示,当放射组学结合临床模型、结合遗传模型以及组合模型时,多变量模型的预后性能得到明显提高。
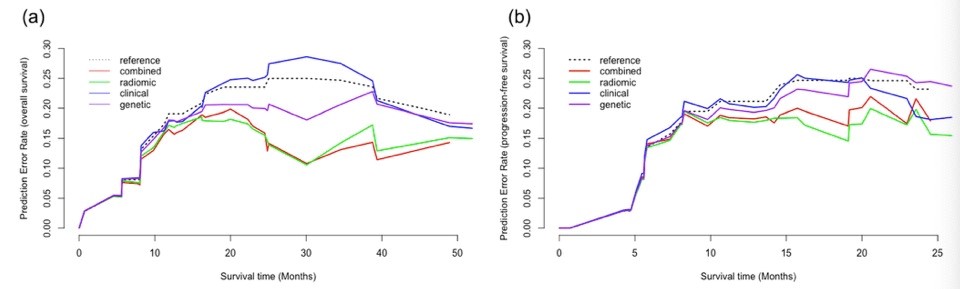
图2(a)总体生存率(b)无进展生存期的多因素Cox模型的预测误差曲线。
本研究证明了使用基于CNN的胶质母细胞瘤多参数分割及放射组学分析进行临床决策的可行性。重要的是,整合了临床、遗传和放射学特征的多变量模型明显提高了预测预后的准确性。本研究为胶质母细胞瘤患者个性化精准医疗方案的制定提供了更多的参考依据。
原始出处:
Yangsean Choi,Yoonho Nam,Jinhee Jang,et al. Radiomics may increase the prognostic value for survival in glioblastoma patients when combined with conventional clinical and genetic prognostic models. DOI:10.1007/s00330-020-07335-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#胶质母细胞#
24
#母细胞瘤#
35
学习一下
59
#患者生存#
28
#生存期#
34
#细胞瘤#
39