心血管疾病(CVD)和包括痴呆在内的脑血管疾病仍然是全球范围内导致死亡和残疾的主要原因,它们具有共同的危险因素。尽管女性和男性有许多共同的危险因素,但是在高血压对脑血管疾病的影响方面,存在着重要的性别差异。
此外,一些心血管疾病的危险因素是妇女特有的。其中的一些与妊娠及其并发症特别相关,如妊娠期高血压疾病(HDP)。患有 HDP 的妇女,特别是妊娠型高血压或先兆子痫的妇女,被建议改变生活方式以降低晚年患病的风险。最近的研究表明,先兆子痫可能与认知障碍甚至痴呆症有关。因此,有研究者认为:认知障碍或痴呆是否应该作为一种潜在的可预防的结果,并纳入心血管疾病指南,而不是围绕降低 HDP 妇女的心血管疾病风险因素。
藉此,鹿特丹大学医学中心的Maria C ADANK等人,系统探究了妊娠期高血压疾病(HDP)与妊娠15年后认知功能损害之间的关系,我纳入了115名有 HDP 病史的妇女和481名有正常血压妊娠史的妇女,并评估他们的认知功能,主要涉及在执行功能、加工速度、言语记忆、运动功能和视觉空间能力等不同的认知领。一个全局认知因子(g-factor)来源于主成分分析,去整体评估认知功能。
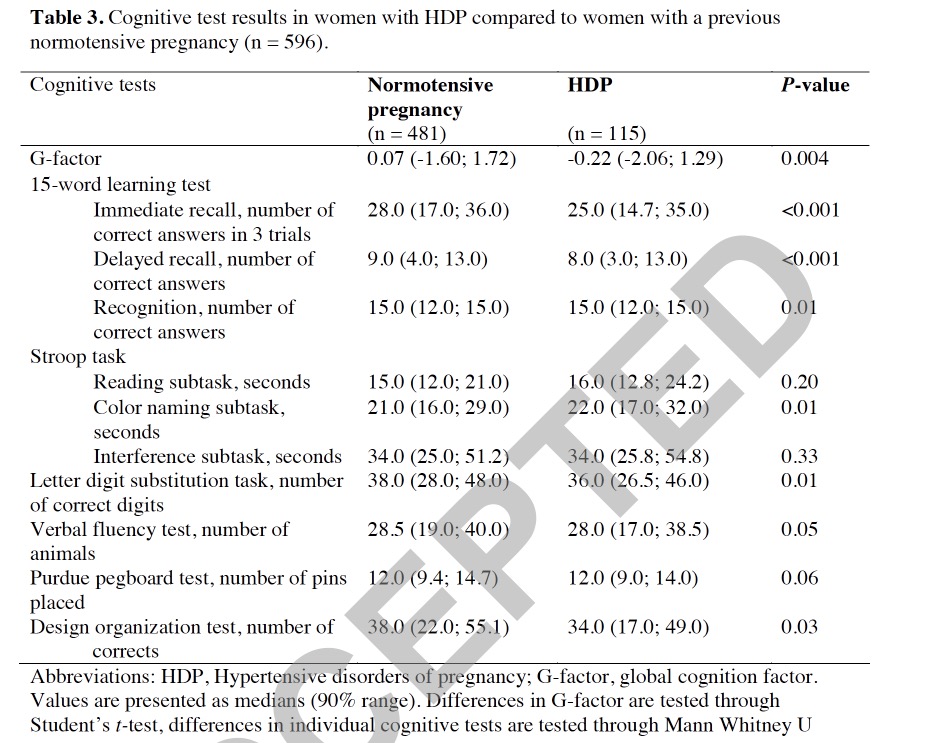
结果发现: HDP 患者中有80例(69.6%)患有妊娠型高血压,35例(30.4%)患有子痫前期。HDP 患者的 g 因子低于有正常血压妊娠史的妇女。HDP 与言语记忆能力呈负相关,主要体现在即刻回忆(- 0.25,95% CI [-0.44-0.06])和延迟回忆(- 0.30,95% CI [-0.50-0.10])减弱。妊娠型高血压的女性在言语学习测试中的表现明显差于血压正常的孕妇。
这个研究的重要意义在于: 妊娠15年后,HDP 病史与较差的工作记忆和语言学习能力独立相关。这种联系主要体现在妊娠型高血压的妇女中。这提示临床医生和经历 HDP 的妇女应该意识到这种风险,并尽可能提前干预。
原文出处:
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#随访研究#
47
#5年随访#
67
学习了
81
#妊娠期#
46
#妊娠期高血压#学习了
118
这也可以
78