JACC:PCI术后5年女性的主要不良心血管事件发生风险更高
2020-04-08 MedSci原创 MedSci原创
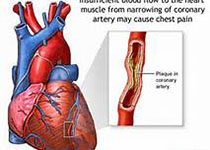
对经皮冠状动脉介入治疗(PCI)后与性别相关的预后研究报道存在相互矛盾的结果。本研究旨在探讨PCI术后5年心血管结局的性别相关风险。
对经皮冠状动脉介入治疗(PCI)后与性别相关的预后研究报道存在相互矛盾的结果。本研究旨在探讨PCI术后5年心血管结局的性别相关风险。
本研究收集了21个随机PCI试验的患者数据,并评估了5年内性别与主要不良心脏事件(心脏死亡、心肌梗死或缺血驱动的靶病变血管重建[ID-TLR])及其单个成分之间的关系。最终,共纳入分析了32877名患者,女性占27.8%。与男性相比,女性年龄更大,体重指数更高,高血压和糖尿病的发生率更高,手术或经皮血管重建的发生率更低。通过血管造影核心实验室分析,女性病变具有更小的病变血管直径和更短的病变长度。术后5年,与男性患者相比,女性患者的MACE、全因死亡率、心源性死亡率和ID-TLR的风险更高。多变量分析发现,女性是MACE和ID-TLR的独立预测危险因素,但不是全因死亡率和心源性死亡率的危险因素。
研究结果显示,经皮冠脉介入术后5年的女性主要不良心血管事件发生风险要高于男性。
原始出处:
Ioanna K et al.Long-Term Outcomes in Women and Men Following Percutaneous Coronary Intervention.JACC.2020 Apr.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PCI术#
43
#血管事件#
38
#JACC#
35
应在同一年龄阶层进行比较才有意义
85
#ACC#
26
#PCI术后#
44
#主要不良心血管事件#
38