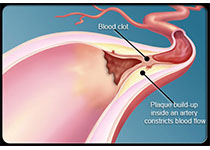
Circulation:将LDL-C浓度控制在70 mg/dL以下或以上对颈动脉粥样硬化斑块发生的影响
2020-08-27 QQY MedSci原创
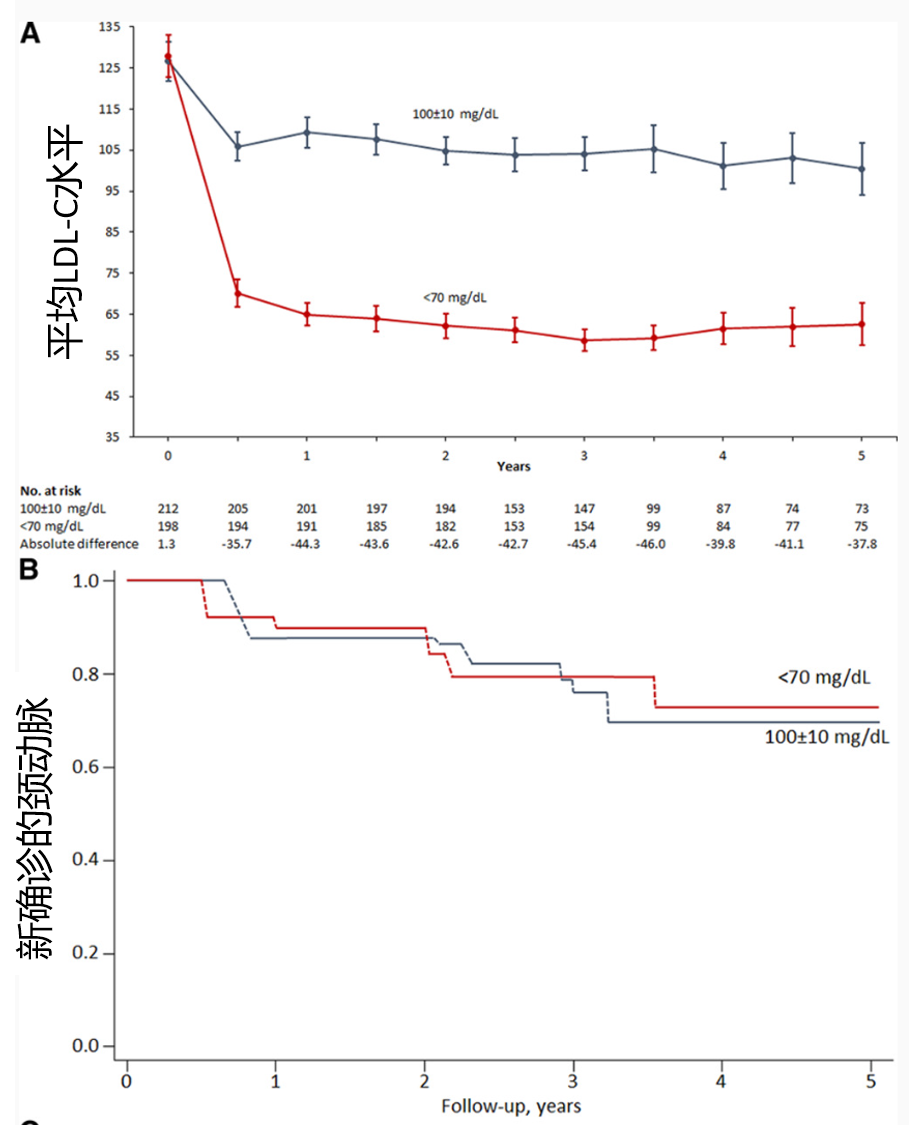
TST试验显示,在2860例伴有脑血管粥样硬化性狭窄的缺血性卒中患者中,将低密度脂蛋白胆固醇浓度控制在70 mg/dL以下可降低主要心血管事件风险。但该策略对颈动脉粥样硬化演变的影响尚不明确
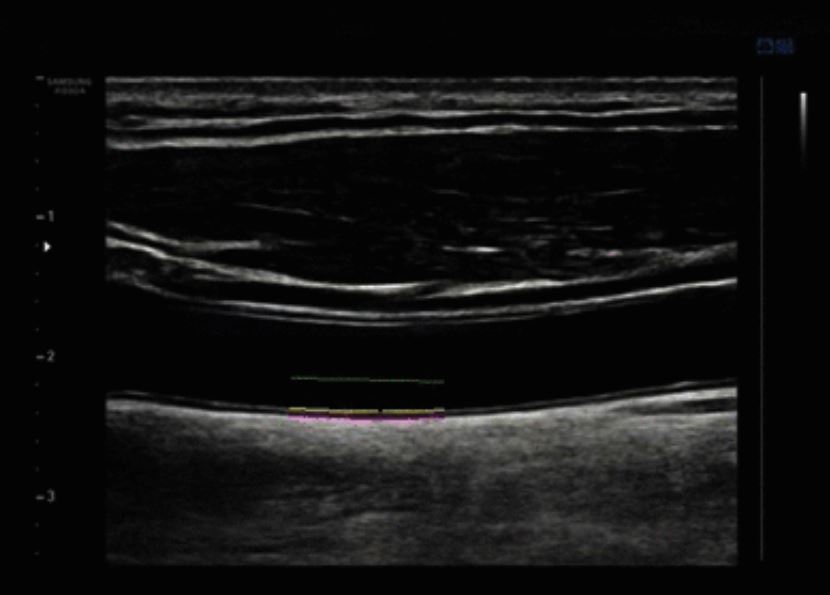
TST-PLUS(治疗卒中至靶斑块超声研究)研究纳入了201例LDL-C<70 mg/dL的患者和212例LDL-C目标为100±10 mg/dL的患者。通过他汀类药物并根据需要添加依折麦布以实现上述目标。在基线,第2、3和5年时,进行颈动脉超声检查。主要结果是新诊断的颈动脉分叉或颈内动脉粥样硬化斑块。
原始出处:
Pierre Amarenco,et al. Carotid Atherosclerosis Evolution When Targeting a Low-Density Lipoprotein Cholesterol Concentration <70 mg/dL After an Ischemic Stroke of Atherosclerotic Origin. Circulation. 2020;142:748–757
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#颈动脉#
41
#粥样硬化#
42
#斑块#
41
#LDL#
38
#颈动脉粥样硬化#
47
#动脉粥样硬化斑块#
0
#浓度#
30
学习学习
93
学到了
89
标记一下回头来看
82