JAMA Oncol:恩杂鲁胺单药治疗可明显降低积极监测的中低危前列腺癌的进展率
2022-06-23 MedSci原创 MedSci原创
在低危和中危局限性前列腺癌患者中,恩杂鲁胺单药治疗的耐受性良好,而且缓解率很高
前列腺癌是美国男性最常见的癌症,70%的新确诊病例仍是局限性病灶。根据国家综合癌症网络治疗指南,主动监测 (AS) 是临床局限性极低风险、低风险或中等风险前列腺癌患者的推荐选择。但目前很少有已发表的研究前瞻性地评估可能延缓接受 AS 的患者前列腺癌进展的药物干预。
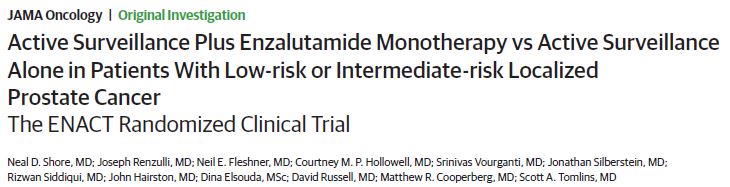
该研究旨在比较恩杂鲁胺单药联合 AS 与单纯 AS 在低危或中危前列腺癌中的效果和安全性。
ENACT研究是一项开放标签、随机化的2期研究,招募了年满18岁、组织学明确诊断的、正在进行 AS 的低危或中危局限性前列腺癌患者,随机(1:1)分至恩杂鲁胺组+AS 组或 AS 组。在治疗的1年和长达两年的随访时间里对患者进行监测。主要终点是病理或治疗性前列腺癌进展。次要终点包括第1年和第2年时的活检阴性率和癌阳性评分比例等。
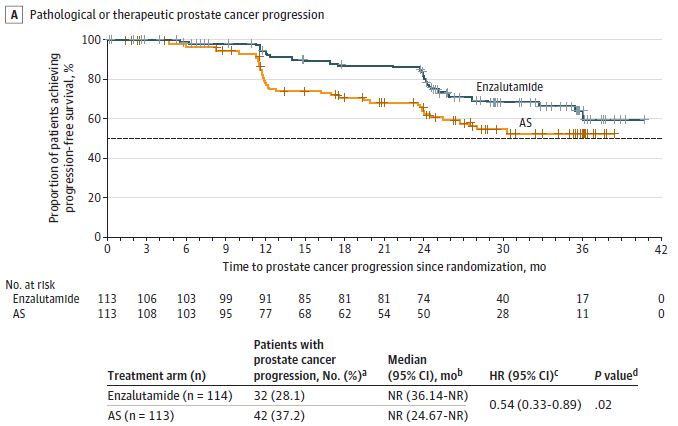
两组患者的进展率
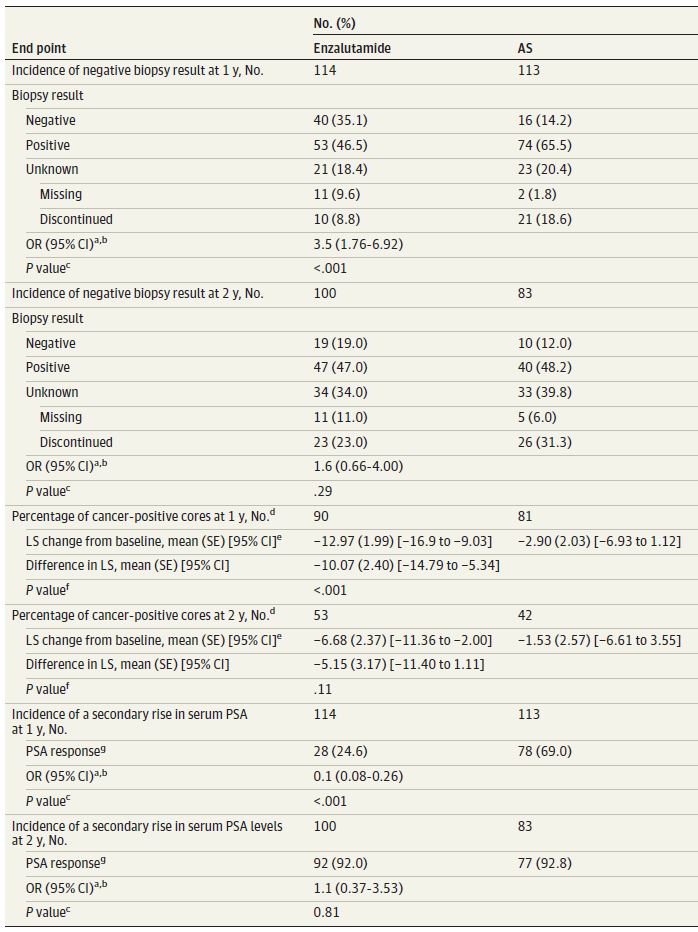
2016年6月至2020年8月,共有227位患者(平均66.1岁)被随机分至恩杂鲁胺+AS 组(n=114)或单 AS 组(n=113)。与单纯 AS 相比,恩杂鲁胺显著降低了前列腺癌进展率(46%,HR 0.54,p=0.02)。第1年时,恩杂鲁胺+AS 组的活检阴性率是单纯 AS 组的3.5倍;而且癌阳性评分比例也显著降低,但第2年时无显著差异。此外,与单纯 AS 相比,恩杂鲁胺治疗还可将 PSA 进展时间延迟6个月之久(HR 0.71,p=0.03)。
次要疗效终点
在恩杂鲁胺治疗期间,最常见的不良反应有疲劳(55.4%)和男性乳房发育症(36.6%)。恩杂鲁胺组有3位患者死亡,在死亡时均未接受研究药物。经判定,无死亡病例与治疗相关。
总之,该研究结果显示,在低危和中危局限性前列腺癌患者中,恩杂鲁胺单药治疗的耐受性良好,而且缓解率很高。恩杂鲁胺或可为接受主动监测的这类前列腺癌患者提供一项新的治疗选择。
原始出处:
Shore ND, Renzulli J, Fleshner NE, et al. Active Surveillance Plus Enzalutamide Monotherapy vs Active Surveillance Alone in Patients With Low-risk or Intermediate-risk Localized Prostate Cancer: The ENACT Randomized Clinical Trial. JAMA Oncol. Published online June 16, 2022. doi:10.1001/jamaoncol.2022.1641.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#单药治疗#
45
#Oncol#
31
#积极监测#
42
学习了
46
学习了,谢谢分享
52
JAMA上文章都是顶级的,谢谢梅斯及时上新
23