Br J Cancer:绝经前后激素水平与浸润性乳腺癌的发病风险相关
2021-05-09 xiaozeng MedSci原创
乳腺癌作为全球女性中最常见的癌症之一,其是激素依赖性的。
乳腺癌作为全球女性中最常见的癌症之一,其是激素依赖性的。在绝经后妇女中,激素替代疗法和肥胖会增加乳腺癌的患病风险。
既往研究显示,某些内源性激素可通过促进细胞增殖和增加随机遗传错误风险以在癌变中起着至关重要的作用。而一些内源激素已被证实与乳腺癌的发病风险相关,然而这些关系的实质尚不完全清楚。
在该研究中,研究人员通过测量英国生物样品库(UK Biobank)在2006–2010年收集的血清以及在2012–13年间收集的重复子样本(N≈5000)中的激素浓度,并通过数据链接确定突发性癌症。该研究旨在评估各激素水平与乳腺癌发病风险之间的关系。
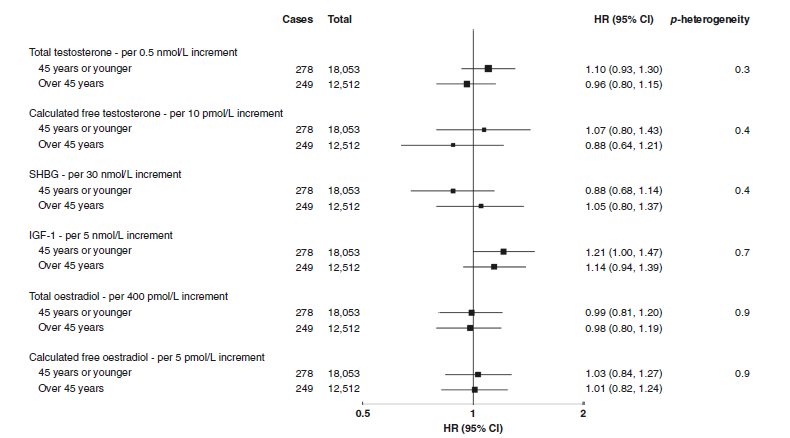
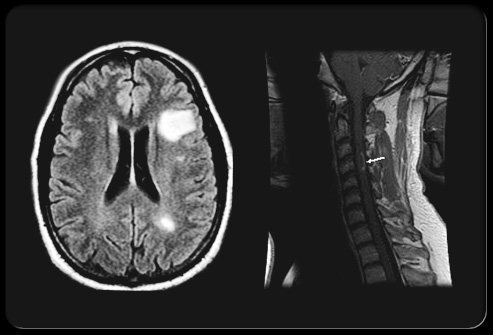
绝经前妇女激素和SHBG水平与侵袭性乳腺癌发病风险的相关性
结果显示,在7.1年的中位随访时间里,30565名绝经前妇女和133294名绝经后妇女分别有527名和2997名被诊断为浸润性乳腺癌。研究人员发现,绝经后妇女的癌症患病风险与睾酮(testosterone)水平呈正相关,而绝经前妇女则无相关性。
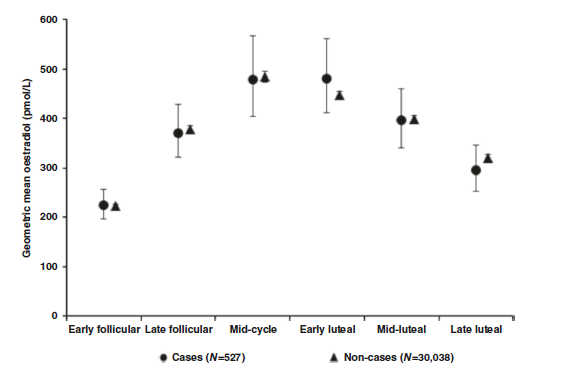
绝经前妇女月经周期各阶段总雌二醇的平均浓度
进一步的研究显示,癌症的发病风险与IGF-1(胰岛素样生长因子1)的水平正相关且与SHBG(性激素结合球蛋白)呈负相关。仅在绝经前妇女中评估到雌二醇与疾病的患病风险无关,但该激素的研究仍较少。
总而言之,这项研究证实了睾酮、IGF-1和SHBG与乳腺癌的发病风险具有相关性,且因绝经状态而出现的异质性与睾酮相关。
原始出处:
Tin Tin, S., Reeves, G.K. & Key, T.J. Endogenous hormones and risk of invasive breast cancer in pre- and post-menopausal women: findings from the UK Biobank. Br J Cancer (16 April 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#激素水平#
47
#绝经前#
35
#绝经#
40
#浸润性乳腺癌#
38
好
72