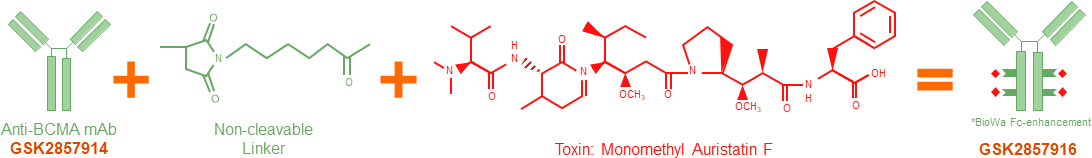
靶向BCMA的ADC药物belantamab mafodotin,获得FDA咨询小组支持治疗复发或难治的多发性骨髓瘤患者
2020-07-15 MedSci原创 MedSci原创
FDA咨询小组周二以12票对0票,支持将葛兰素史克的抗体-药物偶联物(ADC)belantamab mafodotin,用于治疗复发或难治性多发性骨髓瘤(RRMM)患者。
FDA咨询小组周二以12票对0票,支持将葛兰素史克(GlaxoSmithKline)靶向B细胞成熟抗原(BCMA)的抗体-药物偶联物(ADC)belantamab mafodotin,用于治疗复发或难治性多发性骨髓瘤(RRMM)患者。
图片来源:https://mosmedpreparaty.ru/news/19658
GSK一直致力于开发针对接受过至少四项先前疗法(包括抗CD38单克隆抗体、蛋白酶体抑制剂和免疫调节剂)RRMM患者的新疗法。
小组投票之前,FDA最近的一份报告质疑该药物的益处是否超过了关键DREAMM-2试验中观察到的眼毒性风险。他们指出,角膜病变是该研究中最常见的不良事件,总发生率为71%,而44%的患者在2.5 mg/kg剂量下经历了至少一次严重的角膜病变。
关键DREAMM-2研究的数据显示,该药物达到了31%的总缓解率(ORR)。
GSK表示角膜病变可以通过剂量调整来部分控制,并补充说“不会导致永久性角膜溃疡”。
欧洲药品管理局也正在加快审批belantamab mafodotin的市场营销申请。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#FDA咨询小组#
35
#支持治疗#
31
#靶向BCMA#
39
#多发性#
26
#mAb#
30
#BCMA#
35