Cardiovasc Diabetol:钠糖共转运体抑制剂可显著降低T2DM患者的心血管事件风险
2021-07-24 Nebula MedSci原创
启用SGLT-2i与T2DM患者较低的死亡率及心衰和CKD风险相关
关于2型糖尿病 (T2DM) 患者的前瞻性心血管 (CV) 预后试验的结果支持使用钠-葡萄糖共转运蛋白2抑制剂 (SGLT2i) 来降低T2DM患者的心血管事件风险。
CVD-REAL Catalonia试验是一项回顾性的队列研究,采用于2013年至2016年期间日常收集的真实世界的数据,以对比SGLT2i 和其他降糖药 (oGLD)的新使用者之间几种心血管事件的风险。
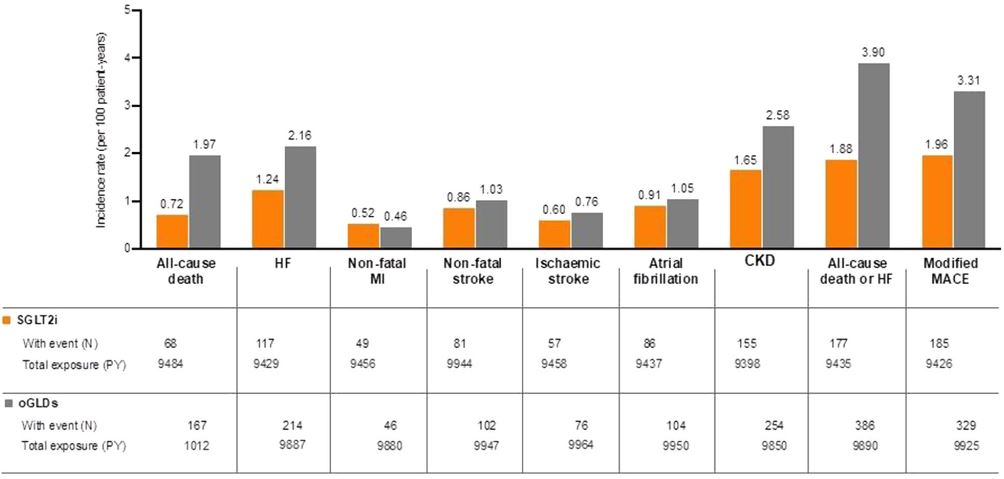
根据倾向性评分以1:1比例纳入了匹配的SGLT2i和oGLD的新使用者。对比了全因死亡率、心衰住院、慢性肾病和校正的主要不良CV事件(MACE;全因死亡率、心肌梗死或卒中)的发生率和风险比(HR)。
两组受试者各种结局的发生情况
经倾向性评分匹配后,每组各纳入了12917位新使用者。约27%的受试者既往有心血管疾病病史。在SGLT2i组,达格列净的暴露时间占60%、恩格列净的占26%、卡格列净的占14%。SGLT2i的使用与较低的心力衰竭(HR 0.59; 95%CI 0.47-0.74; p<0.001)、全因死亡(0.41;0.31-0.54;p<0.001)、全因死亡或心衰(0.55;0.47-0.63;p<0.001)、校正的MACE(0.62;0.52-0.74;p<0.001)和慢性肾病(0.66;0.54-0.80; p<0.001)风险相关。
综上,在这项大型的回顾性观察性研究中,启用SGLT-2i与T2DM患者较低的死亡率及心衰和CKD风险相关。
原始出处:
Real, J., Vlacho, B., Ortega, E. et al. Cardiovascular and mortality benefits of sodium–glucose co-transporter-2 inhibitors in patients with type 2 diabetes mellitus: CVD-Real Catalonia. Cardiovasc Diabetol 20, 139 (2021). https://doi.org/10.1186/s12933-021-01323-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BET#
37
#T2DM患者#
30
#血管事件#
28
#DIA#
30
#ASC#
30
#转运#
34
#抑制剂#
29
#心血管事件风险#
40
学习了,谢谢分享
59
试验是一项回顾性的队列研究。
57