IBD:溃疡性结肠炎患儿全直肠结肠切除术与较高的30天再入院率相关
2021-03-28 MedSci原创 MedSci原创
患者出院后短期内再次住院会给家庭和社会造成巨大的医疗负担,因此,各大医疗机构都将降低30天内再次入院率作为衡量医疗水平的重要指标。
患者出院后短期内再次住院会给家庭和社会造成巨大的医疗负担,因此,各大医疗机构都将降低30天内再次入院率作为衡量医疗水平的重要指标。结直肠手术后的再入院率,在各个疾病中是比较高的,有的医疗机构的再入院率高达30%。目前来说,识别出外科手术患者再入院的危险因素仍然是一个挑战。儿童溃疡性结肠炎(UC)患者经常需要进行全腹结肠切除术(TAC),这部分患者手术后再入院的情况目前还不清楚。因此,本项研究旨在确定接受全腹腔结肠切除术(TAC)的溃疡性结肠炎(UC)患儿的30天再入院率,并确定30天医院再入院的危险因素。

研究人员使用国家外科手术质量改善计划-儿科数据库来识别美国2012年至2017年间接受TAC的小儿UC患者的临床资料,并从住院数据库中收集了患者的手术数据,并使用logistic回归来确定30天再入院率的危险因素。
本项研究最后共纳入了489例行TAC手术的儿童UC 患者的住院数据,其中19.4%的患者在手术出院后30天内再次入院。患者的人口统计学数据和术前实验室检查指标与再次入院的风险无关。调整分析后,包括将直肠切除术纳入的TAC手术方式比单独使用TAC术的30天再入院风险高2倍(OR= 2.4; 95%置信区间为1.1-5.2)
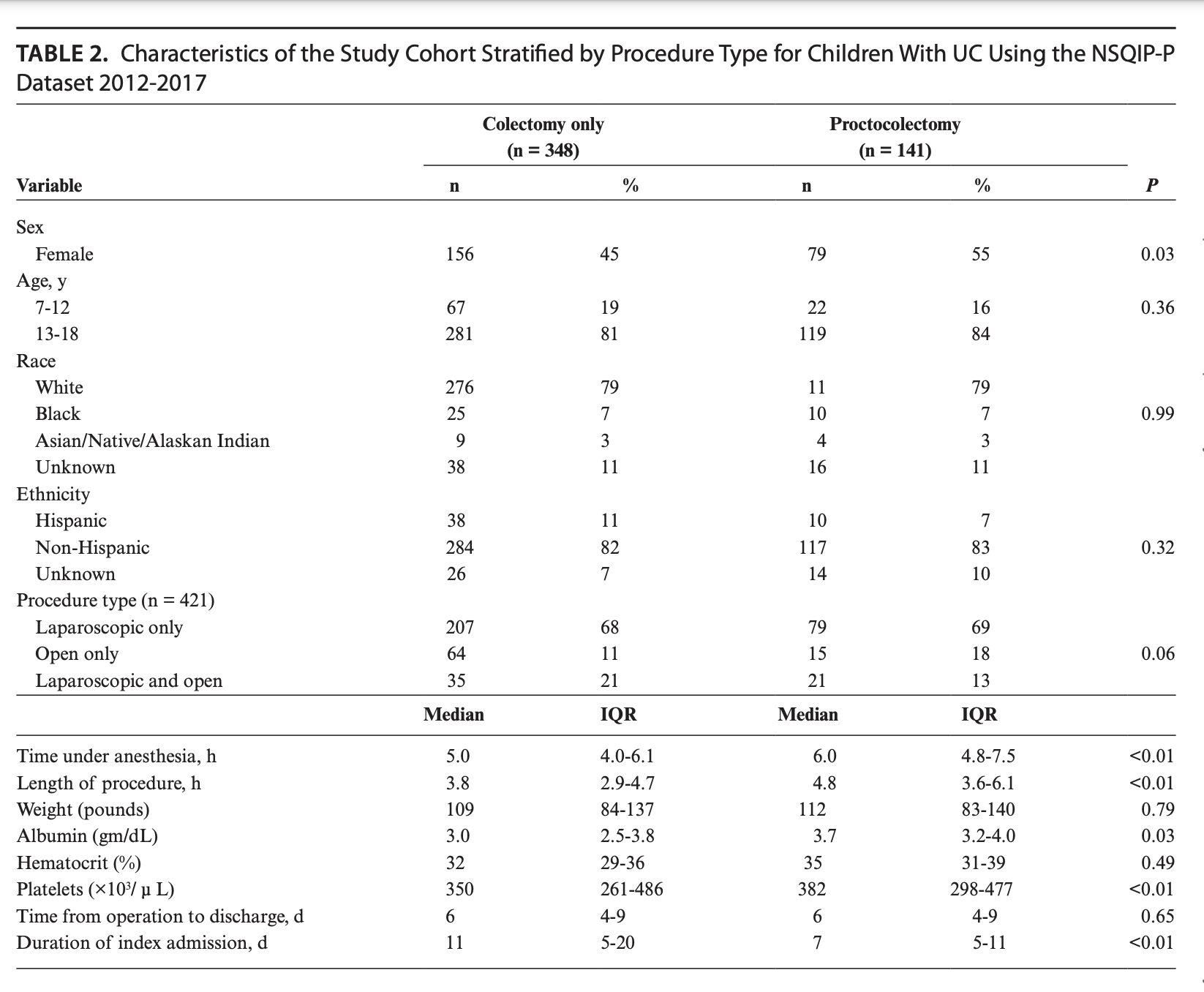
本项研究最后说道:在行结肠切除术的小儿UC住院治疗中,有近20%的患者会在30天内再次入院。值得注意的是,与单独使用TAC相比,将直肠切除的TAC手术方式的再入院率明显更高。
原始出处:
Matthew D Egberg. Et al. Total Abdominal Colectomies With Proctectomy Are Associated With Higher 30-Day Readmission Rates in Children With Ulcerative Colitis. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#30天#
45
#切除术#
30
#结肠切除术#
44
#溃疡性#
23
#IBD#
26
#再入院率#
39
学到了很多东西谢谢老师
64