Cardiovasc Diabetol:得了糖尿病还面临截肢风险! 你注意到下肢的这些变化了吗?
2022-01-12 MedSci原创 MedSci原创
“戒烟、减肥、降血压”三件套,你值得拥有!
外周动脉疾病(PAD)是一种下肢动脉粥样硬化性闭塞性疾病,全世界有数亿人患有这种疾病。其最严重的表现是慢性肢体威胁性缺血(CLTI),定义为存在局部缺血性休息痛、下肢溃疡或坏疽持续时间超过2周。糖尿病患者由于常常合并外周动脉疾病,其发展为CLTI的风险增加,最终导致下肢截肢(LEA)。糖尿病和其他血管危险因素之间的相互作用在影响CLTI风险方面所知甚少。
新加坡是世界上糖尿病(14.2%)和CLTI致LEA发病率最高的国家之一。因此,本研究在新加坡队列中嵌套的主要目的是前瞻性评估糖尿病基线史和CLTI相关LEA发病风险之间的关系。
在基于人群的新加坡华人健康研究中,研究者调查了糖尿病及其与高血压、体重指数(BMI)和吸烟的相互关系,以及CLTI导致的LEA的风险。在招募时对参与者进行了访谈(1993年至1998年),并通过与全国医院数据库的联系,在2017年确定了656例LEA事件病例。使用多变量调整Cox比例风险模型来计算风险比(HRs)和95% CI的相关性。
结果显示,糖尿病患者与非糖尿病患者相比,LEA风险的HR (95% CI)为13.41(11.38–15.79),且随着糖尿病持续时间的延长,风险逐渐增加。高血压和BMI升高分别独立增加了非糖尿病患者的LEA风险,但未增加糖尿病患者的风险。相反,无论糖尿病状况如何,吸烟都会增加约40%LEA的风险。
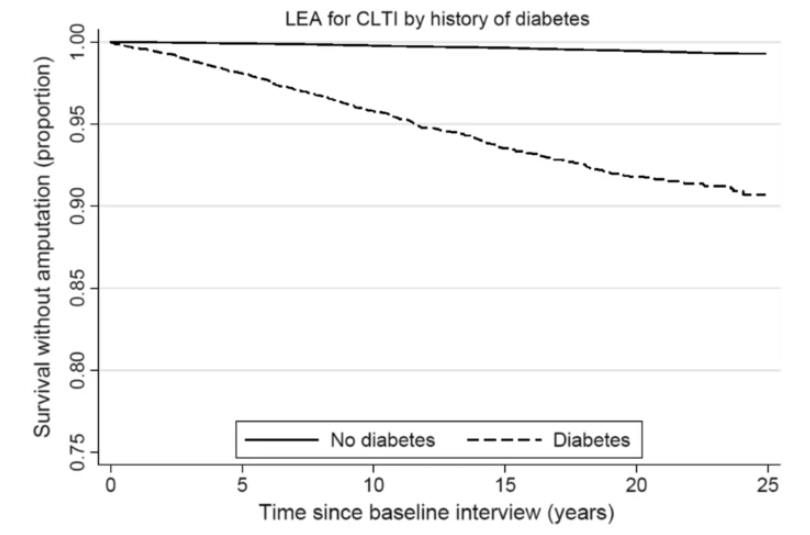
糖尿病史患者下肢截肢治疗慢性威胁肢体缺血(CLTI)的Kaplan-Meier生存曲线
总的来说,虽然糖尿病使LEA发病风险增加了十倍以上,但高血压和BMI增加并没有进一步增加糖尿病患者的LEA发病风险,提示这些危险因素存在共同的机制途径。相比之下,吸烟可能通过另一种途径起作用,因此无论糖尿病状况如何,吸烟都会增加LEA风险。
参考文献:Ying, A.F., Tang, T.Y., Jin, A. et al. Diabetes and other vascular risk factors in association with the risk of lower extremity amputation in chronic limb-threatening ischemia: a prospective cohort study. Cardiovasc Diabetol 21, 7 (2022). https://doi.org/10.1186/s12933-021-01441-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
31
#BET#
27
#DIA#
26
#截肢#
39