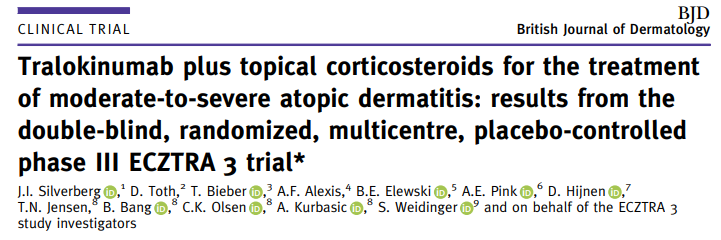
Br J Dermatol:曲妥珠单抗加局部皮质类固醇可有效且安全的治疗中度至重度特应性皮炎
2021-08-16 MedSci原创 MedSci原创
Tralokinumab是一种全人源单克隆抗体,能特异性地中和白细胞介素-13,这是特应性皮炎(AD)的一个关键驱动因素。发表于Br J Dermatol的一项随机双盲试验结果表明,曲妥珠单抗与局部皮
Tralokinumab是一种全人源单克隆抗体,能特异性地中和白细胞介素-13,这是特应性皮炎(AD)的一个关键驱动因素。发表于Br J Dermatol的一项随机双盲试验结果表明,曲妥珠单抗与局部皮质激素(TCS)联合治疗可有效且安全的治疗中度至重度AD患者。
该项双盲、安慰剂+TCS对照的III期试验将纳入的患者按2:1的比例随机分配:皮下曲妥珠单抗300毫克或安慰剂,每2周一次(Q2W),根据需要使用TCS,持续16周。在第16周,使用曲妥珠单抗后,IGA得分达到0/1和/或湿疹面积和严重程度指数(EASI 75)改善75%的患者,按1:1重新随机接受曲妥珠单抗Q2W或每4周(Q4W),根据需要使用TCS,再持续16周。
结果显示,在第16周,与安慰剂相比,曲妥珠单抗组更多的患者达到了IGA 0/1:38.9% vs. 26.2%[差异(95%置信区间):12-4%(2.9-21.9);P = 0.015]和EASI 75:56.0% vs. 35.7%[20.2%(9.8-30.6);P < 0.001]。第16周为曲妥珠单抗应答者的患者中,接受曲妥珠单抗Q2W治疗的患者分别有89.6%和92.5%在第32周分别保持IGA 0/1和EASI 75应答,接受曲妥珠单抗Q4W治疗的患者则分别有77.6%和90.8%。在使用曲妥珠单抗Q2W治疗16周时未达到IGA 0/1和EASI 75的患者中,分别有30.5%和55.8%在第32周达到这些终点。各治疗组的不良事件总发生率相似。
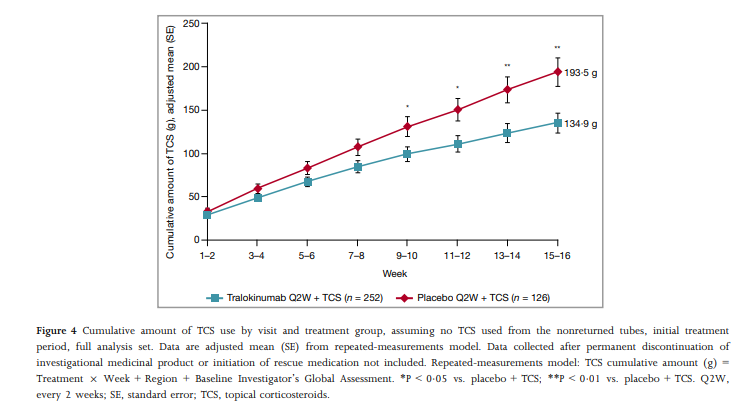
综上,该研究结果表明,Tralokinumab 300 mg联合TCS(根据需要)对中重度AD患者有效,且耐受性良好。
原始出处:
J I Silverberg, et al., Tralokinumab plus topical corticosteroids for the treatment of moderate-to-severe atopic dermatitis: results from the double-blind, randomized, multicentre, placebo-controlled phase III ECZTRA 3 trial. Br J Dermatol. 2021 Mar;184(3):450-463. doi: 10.1111/bjd.19573.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#曲妥珠#
56
#中度至重度#
52
#类固醇#
44
#局部#
40
#中度至重度特应性皮炎#
44
新进展多学习
77
嗯 挺好
78