Front Oncol:真实世界数据探索EGFR 18外显子突变NSCLC患者的治疗策略和预后
2022-01-25 yd2015 MedSci原创
研究表明,对于EGFR 18外显子突变NSCLC患者,1代EGFR TKI联合化疗和阿法替尼可能是最佳治疗方式。
在表皮生长因子受体(EGFR)突变阳性的非小细胞肺癌(NSCLC)患者中,约有3%的患者发生18外显子突变。目前对该亚型患者的适当治疗方案还没有明确。因此,北京协和医院的团队开展了相关研究,目的是研究EGFR 18外显子突变的NSCLC患者对不同治疗方案的疗效。相关结果发表在Frontiers in Oncology杂志上。
研究回顾性分析2014年5月至2020年9月间接受第一代(1G) EGFR-酪氨酸激酶抑制剂(TKI)、第二代(2G) EGFR-TKI阿法替尼、化疗和1G TKI联合化疗作为初始治疗的82例EGFR 18外显子突变患者的临床结局。
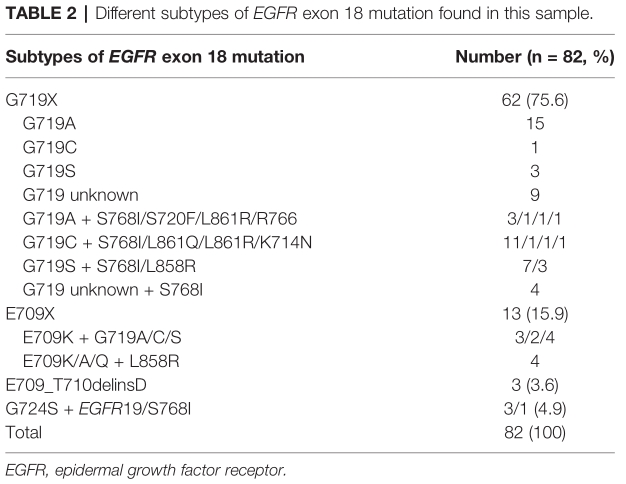
共分析了82例EGFR 18突变的NSCLC患者的治疗和生存结果。中位年龄59岁,女性47例(57.3%)。EGFR 18外显子突变最常见的类型为G719X(75.6%),其次为E709X(15.9%)、E709_T710delinsD(3.6%)和其他亚型(4.9%)。
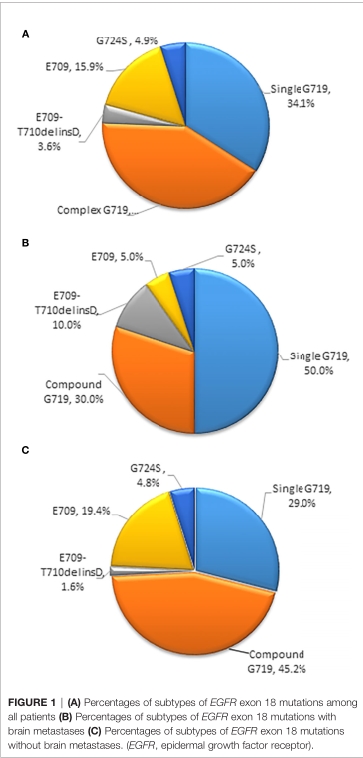
在20例初诊时出现基线神经系统(CNS)转移的患者中,EGFR 18外显子突变亚型最常见的是G719X (n = 16, 80%)和E709_T710delinsD (n = 2, 10%)。
82例患者中,24例患者给予1G EGFR-TKI, 21例患者给予阿法替尼, 22例患者给予化疗,15例患者给予1G EGFR-TKI联合化疗。其中的应答率(ORR)分别为25.0%, 52.4%, 40.9%, 和46.7% (P = 0.276)。 DCRs分别为78.2%, 76.1%, 47.8%, 和86.7%(P = 0.021)。 mPFS分别为7.7 (95% CI, 4.2 11.2)、11.3 (95% CI, 5.6 17.0)、5.0 (95% CI, 2.3 17.7)和11.1个月(95% CI, 5.9 16.4)。
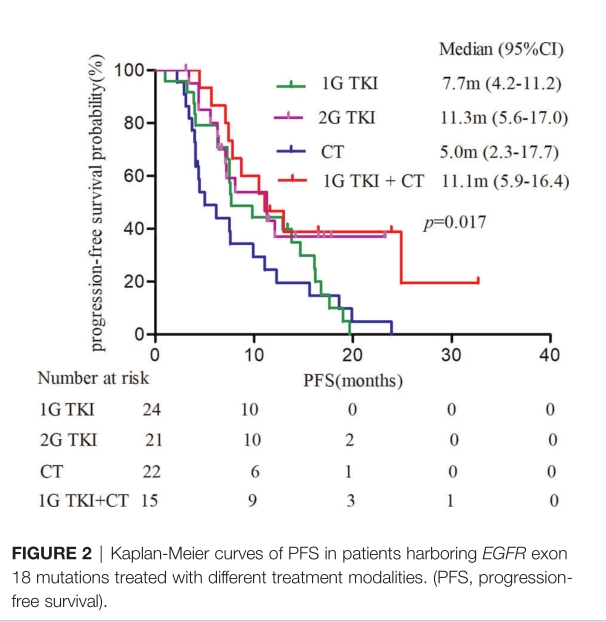
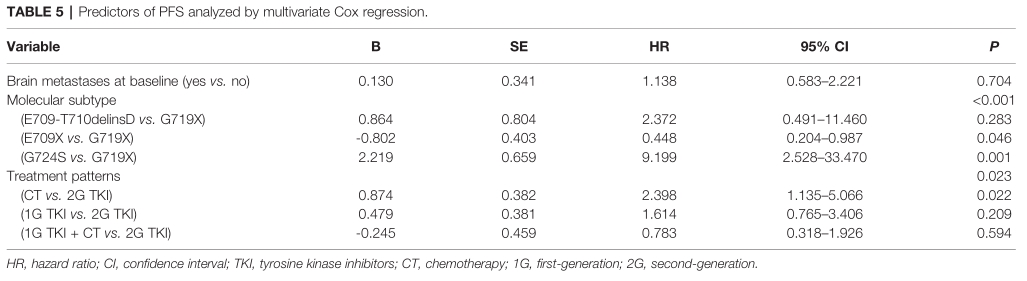
单因素分析显示,EGFR 18外显子突变的晚期NSCLC患者的PFS与分子亚型(P <0.001)和治疗方式(P = 0.023)显著相关。
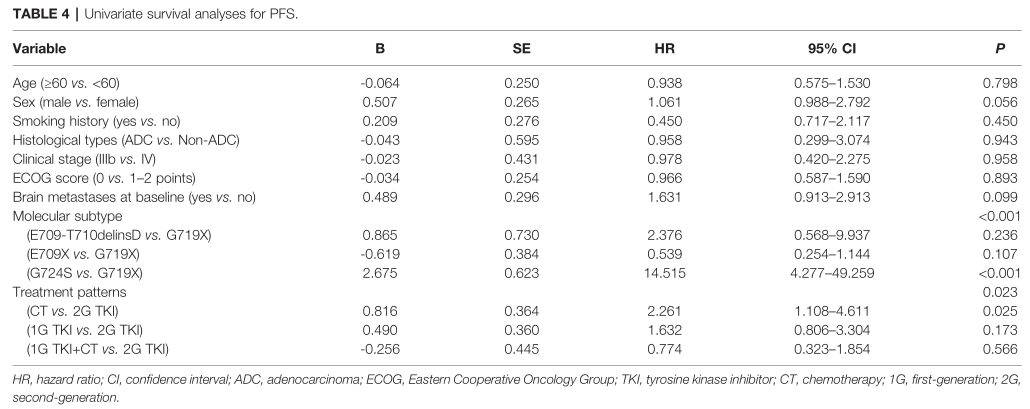
多因素分析证实,EGFR 18外显子的分子亚型和治疗模式是EGFR 18外显子的晚期NSCLC患者PFS的独立预测因素(P<0.05)。
综上,研究表明,对于EGFR 18外显子突变NSCLC患者,1代EGFR TKI联合化疗和阿法替尼可能是最佳治疗方式。
原始出处:
Xu H,Yang G, Li W, LiJ, Hao X, Xing P, Yang Y and Wang Y (2021) EGFR Exon 18 Mutations in Advanced Non-Small Cell Lung Cancer: A Real-World Study on Diverse Treatment Patterns and Clinical Outcomes. Front. Oncol. 11:713483. doi: 10.3389/fonc.2021.713483
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#SCLC患者#
0
#Oncol#
71
学习
53
#真实世界#
40
#NSCLC患者#
41
#GFR#
43
#外显子#
37