Neurology:青少年儿童脑创伤后,白质病变与行为表现相关
2021-06-21 Freeman MedSci原创
Neurology-青少年儿童脑创伤后,白质病变与行为表现相关
弥散MRI(dMRI)彻底改变了无创地观察白质(WM)通路及其在健康和疾病人群中的行为作用的能力。许多dMRI研究表明,年轻的创伤性脑损伤(TBI)患者在一些纤维束中显示出异常的WM组织,如胼胝体。
这些研究还报告了症状和WM组织减少之间的显著的、中度至高度的相关性,如白质破坏的严重程度增加预示着年轻TBI患者的行为表现较差。
人类大脑在发育过程中的可塑性支持学习和适应,但其隐藏的代价可能是对伤害的脆弱性增加。尽管研究结果很有希望,但这些研究受制于样本量(TBI患者的中位数=21),无法测试有关人口学和临床变量对WM组织影响的具体假设。
ENIGMA (Enhancing NeuroImaging Genetics through Meta-Analysis)是一个世界性的合作分析联盟,它利用大型的联合样本来实现足够的力量来解决开放性问题。目前已经建立了ENIGMA小儿中度/重度创伤性疾病(msTBI)工作组,在此调查了创伤性疾病后的WM微结构改变模式。
由于WM指标的变化在受伤后的第一年可能是动态的,根据以前的出版物和队列的研究设计,研究了WM组织在受伤后三个区间的改变。因此假设,在msTBI组中,WM组织的广泛破坏是明显的,关键的人口统计学因素,如年龄和性别,会对结果产生影响。
藉此,美国University of Utah的Emily L Dennis等人,利用ENIGMA探究了:
(1) 小儿中度-重度创伤者,白质组织受到损伤;
(2) 年龄和性别对受伤后白质组织的影响;
(3) 白质组织与神经行为结果之间的关联。
他们纳入了507名儿童和青少年(244名复杂的轻度至重度TBI[msTBI]和263名对照)。患者被分为三个受伤后的时间段:急性/亚急性-<2个月,后急性-2-6个月,慢性-6个月以上。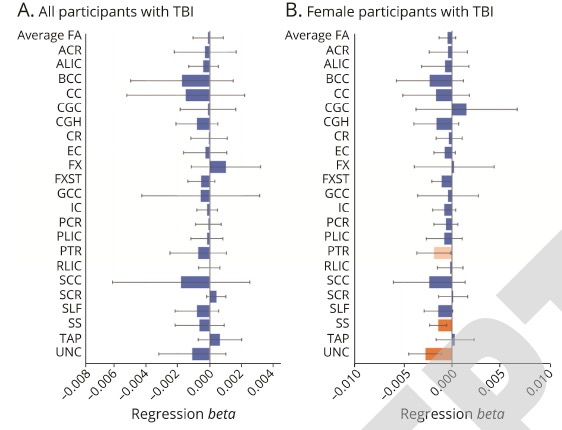
在多个区段和所有受伤后的时间间隔内,WM弥散指标都发生了改变。损伤的严重程度是WM改变程度的一个重要因素,但随着损伤后时间的增加,对dMRI测量的差异解释较少。
性别与组别之间存在相互作用:女性创伤性疾病患者的钩状束各向异性(fractional anisotropy)明显低于对照组(𝞫=0.043),这与父母报告的更多行为问题相吻合(𝞫=-0.0027)。
这个研究的重要意义在于发现了,msTBI后的WM破坏是广泛的、持续的,并受人口统计学和临床变量的影响。
原文出处:
White Matter Disruption in Pediatric Traumatic Brain Injury: Results from ENIGMA Pediatric Moderate to Severe Traumatic Brain InjuryEmily L Dennis, Karen Caeyenberghs, Kristen R Hoskinson, et al. Neurology May 2021, 10.1212/WNL.0000000000012222; DOI: 10.1212/WNL.0000000000012222
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#白质#
30
#Neurol#
38
学习了
66
#创伤#
40
#白质病变#
33