Nat Med:替西帕肽的心血管事件风险评估
2022-02-26 MedSci原创 MedSci原创
与对照组相比,替西帕肽并未增加2型糖尿病参与者发生主要心血管事件的风险。
2型糖尿病导致心血管事件(如冠心病、缺血性卒中、心力衰竭住院(HHF)和血管性死亡)的平均风险高出两倍,与其他已知的危险因素无关。替西帕肽是一种新颖的,每周使用一次的双GIP/GLP-1受体激动剂。目前,它正在开发用于治疗2型糖尿病和肥胖症,但其与心血管结局之间的关联还需要评估。

近日,顶级医学期刊Nature Medicine上发表了一篇研究文章,在这项预先指定的心血管荟萃分析纳入了来自替西帕肽治疗2型糖尿病临床开发计划(SURPASS)的所有七项随机对照试验,受试者采用替西帕肽持续治疗时间至少为26周。
该荟萃分析的预先指定的主要目标是比较合并的替西帕肽组和对照组之间首次发生的四项主要不良心血管事件(MACE-4;心血管死亡、心肌梗死、卒中和需要住院的不稳定型心绞痛)的发生时间。研究人员使用分层Cox比例风险模型,将治疗作为固定效应,将试验水平的心血管风险作为分层因素,用于估计比较替西帕肽与对照的风险比(HR)和置信区间(CI)。
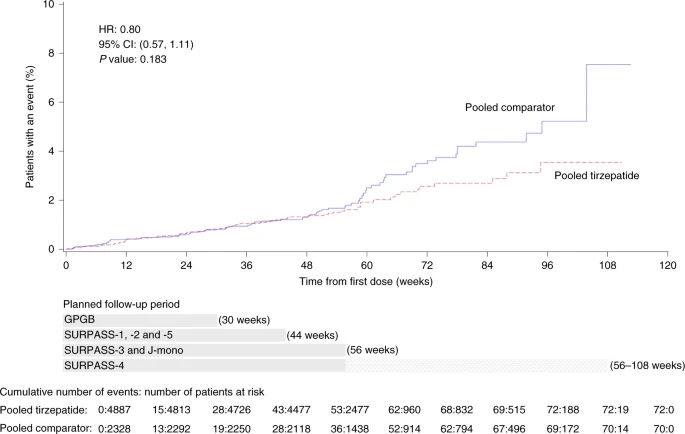
研究人员分析了4887名接受替西帕肽治疗的参与者和2328名对照参与者的数据。总体而言,142名参与者,其中109名来自心血管风险较高的试验,33名来自6项心血管风险较低的试验,至少有一次MACE-4事件。替西帕肽与对照组相比MACE-4的HR为0.80(95%CI为0.57-1.11);心血管死亡为0.90(95%CI为0.50–1.61);全因死亡为0.80(95%CI为0.51–1.25)。研究人员没有观察到任何亚组的效果改变的证据,尽管心血管风险较高的参与者证据更强。
由此可见,与对照组相比,替西帕肽并未增加2型糖尿病参与者发生主要心血管事件的风险。
原始出处:
Naveed Sattar,et al.Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis.Nature Medicine.2022.https://www.nature.com/articles/s41591-022-01707-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
46
#血管事件#
44
学习了
62
#心血管事件风险#
53
#Med#
41