Ann Oncol:转移性激素敏感性前列腺癌的原发癌组织的转录谱特征及与临床预后的相关性
2021-06-17 MedSci原创 MedSci原创
转录组学亚型可指示mHSPC患者预后和适宜的化疗方案
基于总生存期 (OS) 的显著改善,III期CHAARTED试验将前期雄激素剥夺疗法 (ADT) 联合多西他赛 (D) 确定为转移性激素敏感性前列腺癌 (mHSPC) 的标准疗法。目前可预测患者化疗获益和临床预后的标志物/因素尚不明确。
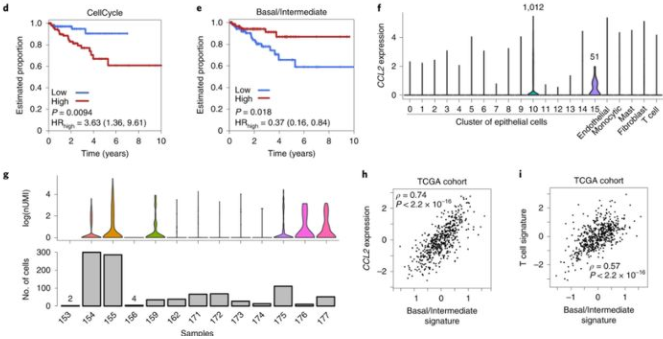
Hamid等人对CHAARTED试验招募的患者于系统治疗前收集原发性前列腺癌(PC)组织进行了全转录组分析,并采用了先验分析计划来测试预定的RNA特征及其与HSPC临床表型和预后的相关性。根据年龄、ECOG 状态、新发转移表现、肿瘤大小和治疗组调整多变量分析 (MVA)。主要终点是OS;次要终点是进展成去势抵抗性前列腺癌前的时间(ttCRPC)。
共纳入了160位原发性PC患者。与局限性PC相比,原发性PC表现出显著不同的转录谱,主要是luminal B(50%)和基底细胞亚型(48%),AR活性低(AR-A)和Decipher风险高。Luminal B亚型与单用ADT的预后较差相关,但Luminal B亚型可从ADT+D治疗中显著受益(OS:HR 0.45,p=0.007);这一点在基底细胞型患者中相反,基底细胞型患者无明显OS获益(HR 0.85,p=0.58),即使是在肿瘤体积较大的患者中。
在多变量分析中,较高的Decipher风险和较低的AR-A均与较差的OS显著相关。此外,较高的Decipher风险与采用ADT+D治疗的患者的OS获益更多相关(HR 0.41,p=0.015)。
综上所述,该研究结果表明,转录组学亚型具有指导mHSPC患者预后和化疗选择的效用,为利用生物标志物指导mHSPC患者选择治疗方案的可能性提供了概念验证。
原始出处:
Hamid A A,Huang H-C,Wang V et al. Transcriptional profiling of primary prostate tumor in metastatic hormone-sensitive prostate cancer and association with clinical outcomes: correlative analysis of the E3805 CHAARTED study.[J] .Ann Oncol, 2021,https://doi.org/10.1016/j.annonc.2021.06.003
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#相关性#
25
#转录#
37
#Oncol#
25
#性激素#
28
#转移性#
25
#敏感性#
35
#临床预后#
26
不错
50
谢谢梅斯分享这么多精彩信息
39
前列腺癌相关研究,学习了,谢谢梅斯
36