JCEM: 缬沙坦改善脂肪组织脂质缓冲能力
2013-04-09 JCEM 丁香园
VAL和安慰剂治疗26周前后,全身和骨骼肌代谢的比较 在糖代谢异常(IGM)的人群,阻断肾素—血管紧张素系统可以降低2型糖尿病的发病率。然而,其潜在的机制有待确定。为了探讨在IGM受试者,血管紧张素Ⅱ1型受体阻断剂缬沙坦(VAL)对骨骼肌脂肪酸(FA)处理的影响,来自荷兰马斯特里赫特大学医学中心Gijs H Goossens教授及其团队进行了一项研究,该研究发现缬沙坦可以改善脂肪组织的脂质缓冲能
在糖代谢异常(IGM)的人群,阻断肾素—血管紧张素系统可以降低2型糖尿病的发病率。然而,其潜在的机制有待确定。为了探讨在IGM受试者,血管紧张素Ⅱ1型受体阻断剂缬沙坦(VAL)对骨骼肌脂肪酸(FA)处理的影响,来自荷兰马斯特里赫特大学医学中心Gijs H Goossens教授及其团队进行了一项研究,该研究发现缬沙坦可以改善脂肪组织的脂质缓冲能力。该研究结果在线发表在2013年4月3日的美国《临床内分泌代谢杂志》(The Journal of clinical endocrinology & metabolism)上。
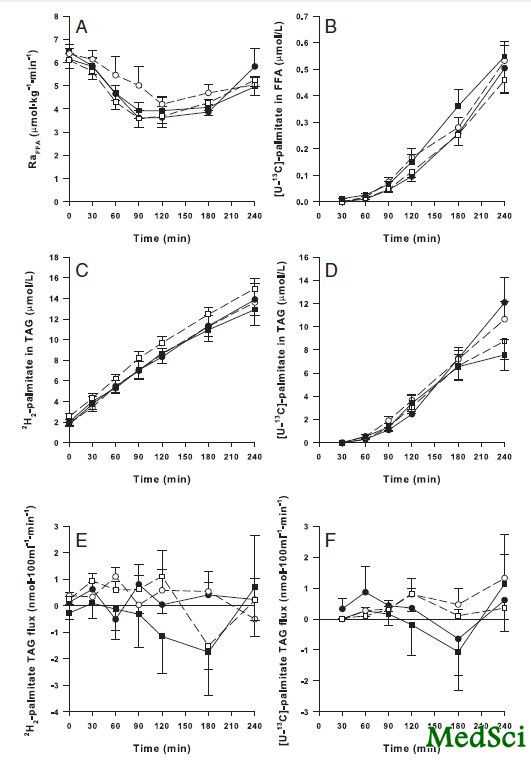
该研究是在马斯特里赫特大学医学中心进行的一项随机、双盲、安慰剂对照试验。在26例IGM受试者中,评估基线和VAL或安慰剂治疗26周后的空腹和餐后的骨骼肌脂肪酸处理。空腹和餐后的骨骼肌脂肪酸处理通过前臂平衡技术联合稳定同位素标记的棕榈酸酯确定。2H2-棕榈酸酯静脉输注标记循环内的内源性甘油三酯(TAG)和游离脂肪酸(FFA),U-13C-棕榈酸酯混入高脂混合餐(2.6MJ,61%能量来自脂肪)标记乳糜微粒TAG。使用肌肉活检标本确定肌注TAG、二酰甘油(DAG)、FFA和磷脂成分,他们的分数合成率和饱和度,以及氧化基因mRNA表达。
该研究结果表明,VAL降低肌注TAG和DAG的饱和分数,但不影响净肌肉摄取2H2-棕榈酸酯,极低密度脂蛋白2H2-TAG和乳糜微粒U-13C-TAG,以及肌肉mRNA的表达。通过循环U-13C-棕榈酸酯判断,VAL降低FA溢出,FFA显现率以及倾向于降低乳糜微粒TAG浓度。
该研究发现,VAL治疗26周减少骨骼肌TAG和DAG的储存饱和度,提示改变FA的肌间脂质分配。VAL诱导餐后FA溢出、内源性脂解和乳糜微粒TAG浓度的减少,提示改善脂肪组织脂质缓冲能力。
与缬沙坦相关的拓展阅读:
- KYOTO HEART研究:缬沙坦对伴CKD高血压者有益
- 缬沙坦再添亚洲人群心脑血管保护新证据
- KYOTO HEART 研究:高危高血压患者应用缬沙坦对心血管事件的影响:KYOTO HEART 研究的最新分析
- JIKEI HEART:在日本缬沙坦对冠状动脉疾病患者的作用 更多信息请点击:有关缬沙坦更多资讯

The Effects of Long-Term Valsartan Treatment on Skeletal Muscle Fatty Acid Handling in Humans With Impaired Glucose Metabolism
Context
Blocking the renin-angiotensin system reduces the incidence of type 2 diabetes mellitus in humans with impaired glucose metabolism (IGM). Nevertheless, underlying mechanisms remain to be established.
Objective
The purpose of this study was to investigate the effects of the angiotensin II type 1 receptor blocker valsartan (VAL) on skeletal muscle fatty acid (FA) handling in subjects with IGM.
Design/Setting
This was a randomized, double-blind placebo-controlled trial at Maastricht University Medical Center.
Intervention/Main Outcomes/Participants
Fasting and postprandial skeletal muscle FA handling were assessed at baseline and after 26 weeks of treatment with VAL or placebo in 26 subjects with IGM. Fasting and postprandial skeletal muscle FA handling were determined by combining the forearm balance technique with stable isotopes of palmitate. [2H2]-Palmitate was infused iv to label endogenous triacylglycerol (TAG) and free fatty acid (FFA) in the circulation, and [U-13C]-palmitate was incorporated in a high-fat mixed meal (2.6 MJ, 61% energy from fat) to label chylomicron TAG. Muscle biopsy samples were taken to determine im TAG, diacylglycerol (DAG), FFA, and phospholipid contents, their fractional synthetic rates and degree of saturation, and mRNA expression of oxidative genes.
Results
VAL decreased saturation of im TAG and DAG fractions but did not affect net muscle uptake of [2H2]-palmitate, very low-density lipoprotein ([2H2])-TAG and chylomicron ([U-13C])-TAG, and muscle mRNA expression. VAL decreased FA spillover, as estimated by circulating [U-13C]-palmitate, and FFA rate of appearance and tended to decrease chylomicron TAG concentrations.
Conclusions
VAL treatment for 26 weeks decreased saturation of skeletal muscle TAG and DAG stores, suggesting altered intramuscular lipid partitioning of FA. The VAL-induced reduction in postprandial FA spillover, endogenous lipolysis, and chylomicron TAG concentrations indicate improved adipose tissue lipid buffering capacity.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCEM#
22
#缓冲能力#
31
#JCE#
31
#脂肪组织#
34
#缬沙坦#
31