JAHA:不同类型心脏手术后急性肾脏损伤的长期结局
2021-04-21 MedSci原创 MedSci原创
与其他心脏手术相比,主动脉手术引起D-AKI的发生率更高,但肾脏恢复更好,短期预后更好,长期透析的发生率更低。
需要透析的急性肾损伤(D-AKI)是心血管外科手术的主要并发症,其会导致患者较差的预后。但是,尚未完全明确D‐AKI在不同类型心脏手术患者中的发生率和影响。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员从台湾国家健康保险研究数据库中确定了2004年7月1日至2013年12月31日期间接受心血管手术的患者,并将患者分为D-AKI组(n=3089)和非D-AKI组(n=42151)。该研究的结局是全因死亡率和主要不良肾脏事件。
研究人员发现D-AKI组的长期预后较非D-AKI组更差(严重不良肾脏事件的风险比[HR]为3.89;95%CI为3.79-3.99;全因死亡率HR为2.89;95%CI为2.81–2.98)。
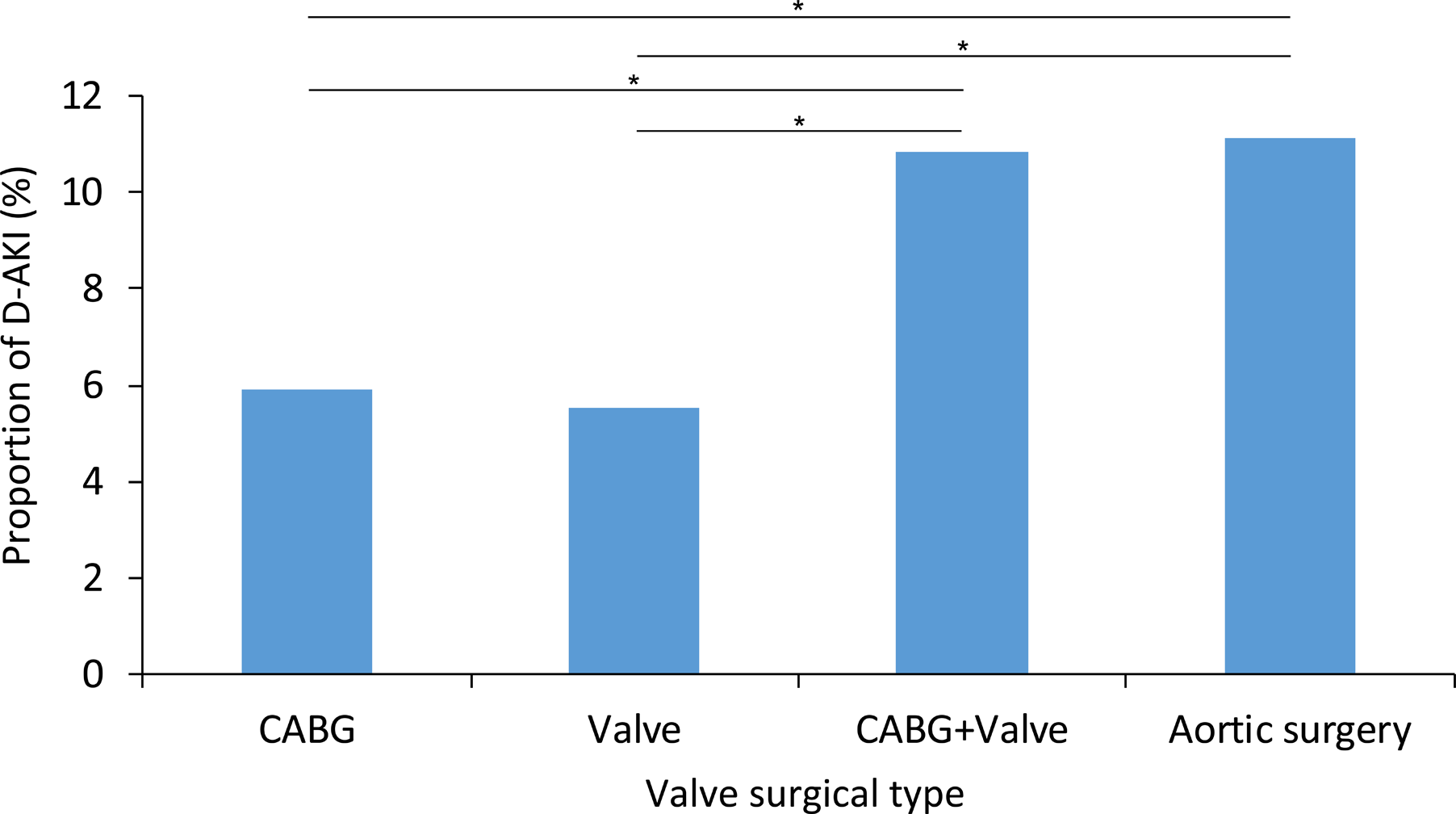
接受主动脉手术的患者比其他类型的手术具有更高的D-AKI风险,但他们康复的几率更高。从D-AKI中恢复的患者的长期透析率在进行主动脉手术的患者中也最低。在伴有D‐AKI的所有类型心脏手术患者中,接受心脏瓣膜手术的患者全因死亡率最高(HR为6.04;95%CI为5.78-6.32)。
由此可见,与其他心脏手术相比,主动脉手术引起D-AKI的发生率更高,但肾脏恢复更好,短期预后更好,长期透析的发生率更低。
原始出处:
Jia‐Jin Chen.et al.Long‐Term Outcomes of Acute Kidney Injury After Different Types of Cardiac Surgeries: A Population‐Based Study.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.019718
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












心
12
#不同类型#
42
#AHA#
32
#长期结局#
34
#损伤#
36
学习了,谢谢
61
在伴有D‐AKI的所有类型心脏手术患者中,接受心脏瓣膜手术的患者全因死亡率最高
64
学习!
69
学习了,谢谢
56
学习了、涨知识了!
57