Nat BME :基于CRISPR的移植排斥反应监测方法
2020-07-04 Medsci原创 Medsci原创
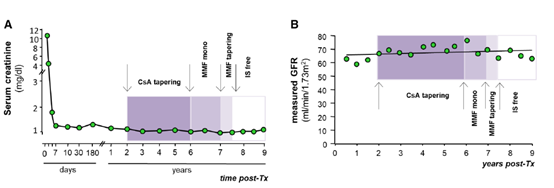
在器官移植中,感染和排斥反应是移植物丢失的主要原因。它们是由免疫抑制的净状态联系在一起的。为了早期诊断和治疗这些疾病,并改善患者的长期预后,需要改进移植后患者的监测策略。
本文介绍了一种基于CRISPR-Cas13的快速、廉价的检测方法,这种方法能够准确地检测患者血液和尿液中的BK多瘤病毒DNA和巨细胞病毒DNA,以及CXCL 9信使RNA,在发生急性肾移植排斥反应的患者尿液中检测到了较高水平的BK多瘤病毒DNA和巨细胞病毒DNA。通过简单的可视化,这种方法可以对常见病毒感染和移植排斥反应进行移植后监测,并应有助于移植后的点对点监测。
CRISPR和Cas免疫系统用于检测核酸,这种快速,经济有效的DNA和RNA检测在各种类型的样本具有良好的敏感性和特异性,本文,作者应用并优化了CRISPR–Cas13特异性(SHERLOCK)技术,用于诊断,检测与肾移植受者高度相关的生物标志物。
作者开发了基于CRISPR的巨细胞病毒(CMV)和BK多瘤病毒(BKV)感染的诊断工具,对100多份来自BKV和CMV感染者的临床标本进行了广泛的病毒载量检测,结果显示诊断准确率很高。进一步将SHERLOCK的能力扩展到检测人CXCL9 mRNA(指示肾移植受者排斥反应的生物标志物)。
方法:作者从感染患者和未感染对照患者的血液和尿液中分离出DNA。随后,将改进版的SHERLOCK协议应用于BKV和CMV检测。用等温重组酶聚合酶扩增(RPA)扩增BKV和CMV的保守区。将T7启动子序列整合到前向引物中,可以使用T7聚合酶进行后续的体外RNA转录。用CRISPR引导RNA(crRNA)与RPA产物的28个核苷酸互补,将Cas13从wadei瘦肉杆菌(LwaCas13a)导入靶序列。对靶的检测导致Cas13激活,随后伴随着一个带有猝灭荧光团的寡核苷酸的侧方裂解,该荧光团与患者样本中靶的初始浓度相关。
为了确定BKV基因组中的保守区域,从NCBI获得的所有菌株进行了比对,并将重点放在所有菌株中序列同源性超过95%的目标区域。接下来,测试了12对不同的引物和3个crRNAs检测BKV基因STA、VP2和VP3的能力。确定了一对特异于小T抗原(STA)的crRNA-引物对,允许检测低阿氏量范围(0.3μaM)的美国型培养物收集(ATCC)定量合成BKV标准品(Dunlop株),代表所用分析体积中的单分子检测。
结论:这项工作展示了CRISPR–Cas13在肾移植排斥反应和机会性感染检测中的应用。这项技术可以应用于其他实体器官移植以及免疫介导的肾脏疾病,如狼疮性肾炎。该方法具有成本低、使用方便、快速等优点,可实现频繁检测和早期诊断。
Kaminski, M.M., Alcantar, M.A., Lape, I.T. et al. A CRISPR-based assay for the detection of opportunistic infections post-transplantation and for the monitoring of transplant rejection. Nat Biomed Eng 4, 601–609 (2020). https://doi.org/10.1038/s41551-020-0546-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#监测方法#
35
#Nat#
32
#排斥#
39
#CRISPR#
34
#排斥反应#
0
!
110