内镜下治疗腰椎间盘脱出合并邻近节段黄韧带囊肿1例
2019-11-19 于江涛 陶志强 范少勇 中国矫形外科杂志
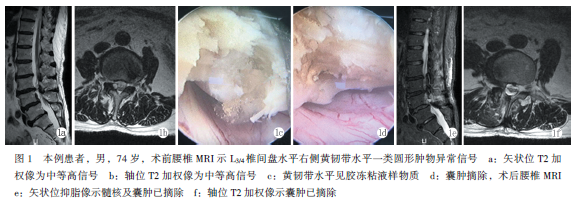
患者,男,74岁;主诉因“腰痛及右下肢麻胀痛4个月余,加重1周”入院。专科检查:L3/4棘突旁压痛阳性,右小腿内外侧感觉稍减退,四肢肌力正常,右直腿抬高试验30°(+),双侧膝腱、跟腱反射正常,病理反射未引出。术前腰腿疼痛视觉模拟评分7分。辅助检查:MRI显示:L4/5椎间盘向右后上方脱出及L3椎管右后方肿物(图1a)。入院诊断:(1)腰椎管狭窄症;(2)L4/5椎间盘脱出症;(3)L3硬膜外椎管
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#黄韧带囊肿#
32
#黄韧带#
42
#内镜#
35
#腰椎#
28
#囊肿#
30
#韧带#
23
#腰椎间盘#
53