AGING CELL:肝骨素对于预防非酒精性脂肪肝是必须的
2020-07-21 MedSci原创 MedSci原创
在肝脏正常的个体中,研究人员观察到血清OPN水平与年龄的增加呈正相关。然而,在非酒精性脂肪肝患者中,这种与年龄的相关性却不存在。
骨质疏松素(OPN)是一种衰老相关的分泌表型因子,在非酒精性脂肪性肝病(NAFLD)患者中增加。细胞衰老与年龄依赖性肝硬化有关。
因此,研究人员对OPN在年龄相关肝硬化中的作用进行了探究。为此,他们使用了人类血清样本、衰老的动物模型和诱导衰老的细胞系,测定了代谢通量、脂质和蛋白质浓度。
在肝脏正常的个体中,研究人员观察到血清OPN水平与年龄的增加呈正相关。然而,在非酒精性脂肪肝患者中,这种与年龄的相关性却不存在。
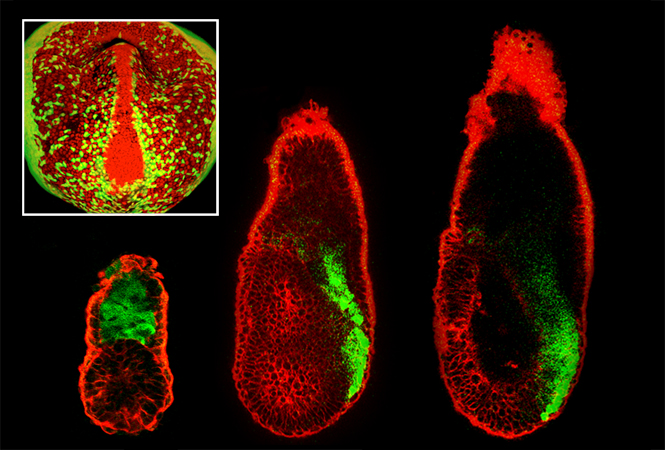
在野生型(WT)小鼠中,血清和肝脏OPN在10月龄(m)时与肝脏p53水平一起增加,并在20月龄时保持升高。与WT肝细胞相比,10月龄OPN缺失(KO)小鼠的肝细胞中肝脏衰老的标志物与甘油三酯(TG)的合成和浓度增加。10月龄OPN-KO小鼠肝脏中衰老和脂质代谢的这些变化与78 kDa葡萄糖调节蛋白(GRP78)的减少,ER应激的诱导,以及脂肪酸合成酶和CD36水平的增加有关。
衰老细胞中OPN的缺失也使GRP78、细胞内TG的积累和CD36水平的增加减少。
在20月龄小鼠中,OPN丢失导致肝纤维化增加。
最后,研究人员表明,OPN在体外和体内的表达受p53的调控。
总之,OPN缺失会导致衰老过程中更早的细胞衰老、ER应激和TG积累。p53-OPN轴是抑制年龄相关性肝硬化发生所必需的。
原始出处:
Beatriz Gómez‐Santos et al. Liver osteopontin is required to prevent the progression of age‐related nonalcoholic fatty liver disease, AGING CELL (2020). DOI: https://doi.org/10.1111/acel.13183
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#酒精性#
27
#酒精性脂肪肝#
30
#CEL#
35
#Cell#
26
#非酒精性#
31
感谢分享
87