J Thorac Oncol:EGFR 突变NSCLC脑膜转移患者TKI抑制剂进展后鞘内注射培美曲塞联合地塞米松的疗效和安全性
2021-07-19 yd2015 MedSci原创
该研究表明50mg培美曲塞鞘内注射治疗TKI治疗进展的EGFR 突变NSCLC脑膜转移患者毒性较低,并且有较好的临床缓解。
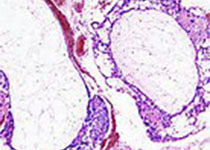
大约3%-5%的晚期非小细胞肺癌(NSCLC)患者会出现脑膜转移。由于血脑屏障,伴有脑膜转移的患者预后较差,中位生存大约3个月。鞘内注射化疗药物是其常用的治疗方式之一。培美曲塞是肺腺癌常用的化疗药物。但是其用于鞘内注射的治疗不明确。因此,来自我国哈尔滨医科大学的研究团队开展了一项I/II期临床研究(Unique Identifier: ChiCTR1800016615),评估NSCLC脑膜转移患者,鞘内注射培美曲塞(IP)的最大耐受剂量(MTD),以及推荐剂量(RD)用于治疗的疗效和安全性。相关结果发表在Journal of Thoracic Oncology杂志上。
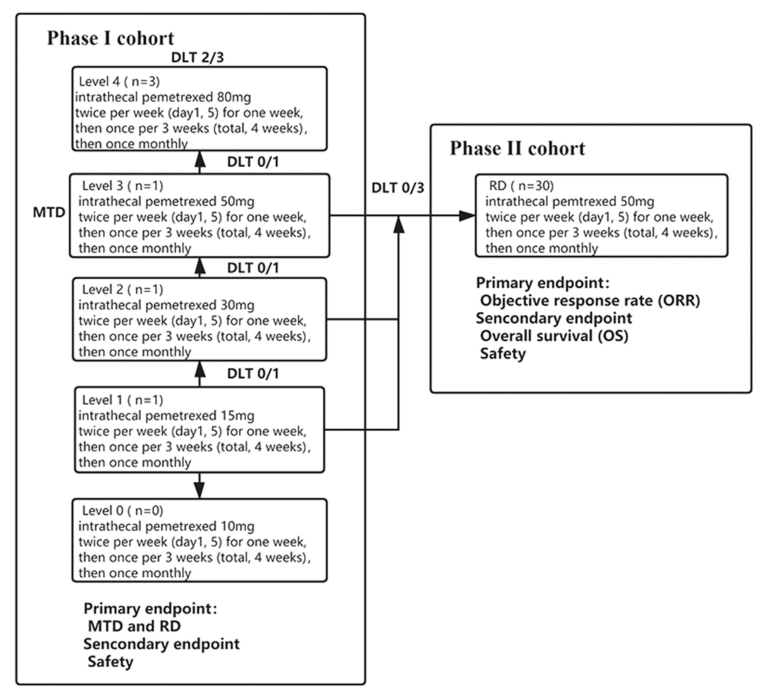
该研究是前瞻性、开放标签、单臂的I/II期研究。纳入EGFR突变阳性NSCLC伴有脑膜转移(LM)使用TKI抑制剂治疗失败的患者。I期研究中使用培美曲塞的剂量为15 mg 至80 mg,以确定推荐治疗的剂量。II期研究使用推荐剂量(RD)进行治疗。主要研究终点为治疗疗效(使用缓解率评估),次要研究终点是OS和安全性。
研究概况
I期研究确定培美曲塞的推荐剂量(RD)为50mg。30例患者纳入II期研究中,包括16例男性和14例女性。15例患者初始发现脑脊液(CSF)细胞学阳性;19例患者MRI阳性,11例为MRI阴性。所有患者经检测为EGFR突变阳性,并且接受TKI抑制剂治疗。其中27例患者接受一代TKI治疗,25例接受过奥希替尼治疗。所有患者接受多线治疗失败(≥3),包括系统化疗,分子靶向治疗和鞘内化疗。
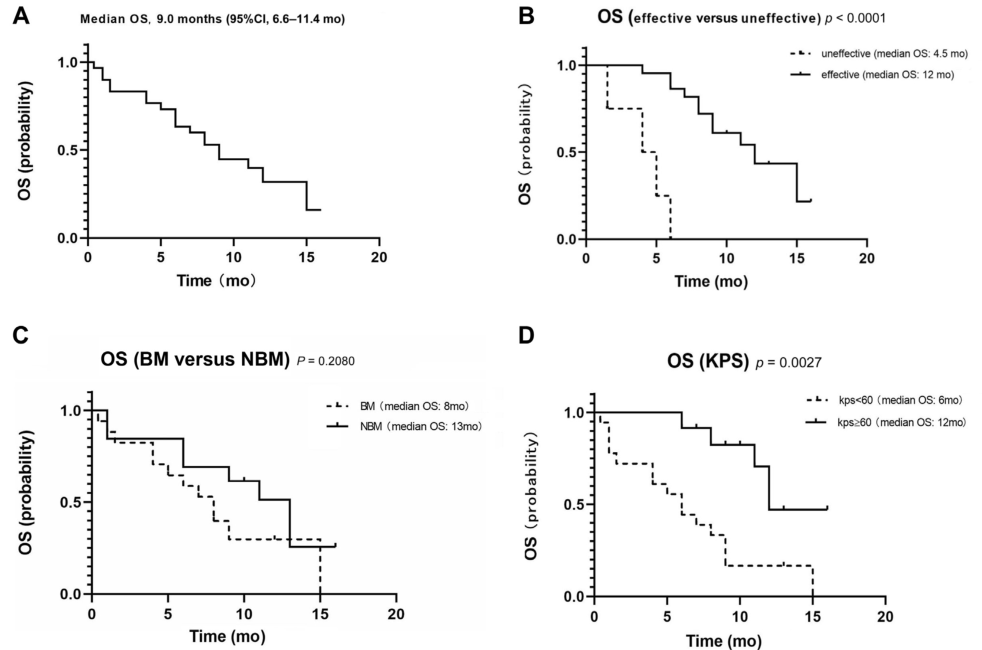
中位随访时间11个月,中位OS为9个月(n =30, 95% CI: 6.6–11.4)。26例患者可进行疗效评估,临床缓解率为84.6%(22 of 26),其中2例患者达到完全缓解(CR)(OS:8.0 –未达到, 中位: 未到达),13例得到显著缓解(OS: 6.0–16.0, 中位: 12.0个月),7例患者达到部分缓解(PR)(OS:4.0–15.0, 中位: 9.0个月),3例患者疾病稳定(SD)(OS: 4.0–6.0, 中位: 5.0个月), 1例患者疾病进展(PD) (OS: 1.5个月)。总的来说,22例取得应答(OS: 4.0–16.0, 中位: 12.0个月),而4例取得稳定和疾病进展(OS: 1.5–5.0, 中位: 4.5个月)。

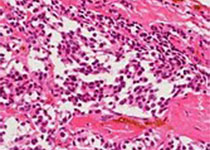
疗效评估
亚组分析发现,伴有脑转移和不伴有脑转移患者的中位OS分别为8个月和11个月,但是没有显著统计学差异(p=0.2058);高KPS评分患者(KPS ≥ 60, 中位OS: 12.0个月)较低KPS评分患者(KPS < 60, 中位 OS: 6.0个月)获得生存获益(p=0.0027)。同样,临床应答患者较不应答患者取得OS获益(p < 0.0001)。
OS
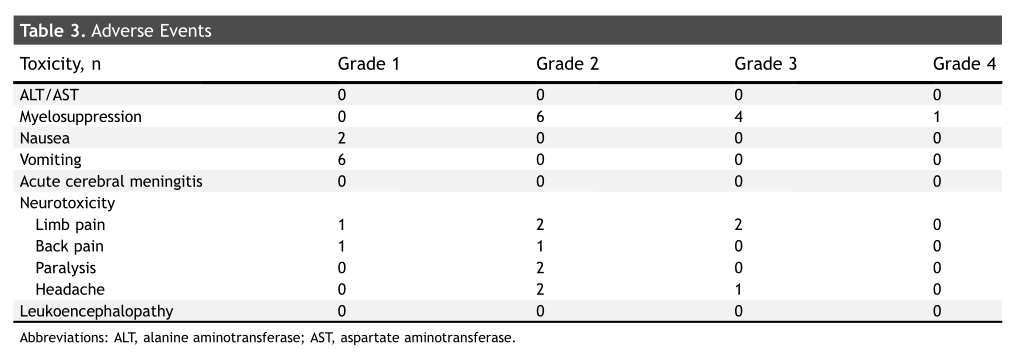
大多数不良事件(AEs)是轻度的。任何级别的常见AEs为骨髓抑制(n=9,30%),经过对症治疗后可恢复正常。
不良事件
综上,该研究表明50mg培美曲塞鞘内注射治疗TKI治疗进展的EGFR 突变NSCLC脑膜转移患者毒性较低,并且有较好的临床缓解。
原始出处:
Fan C, Zhao Q, Li L, et al. Efficacy and Safety of Intrathecal Pemetrexed Combined With Dexamethasone for Treating Tyrosine Kinase Inhibitor-Failed Leptomeningeal Metastases From EGFR-Mutant NSCLC-a Prospective, Open-Label, Single-Arm Phase 1/2 Clinical Trial (Unique Identifier: ChiCTR1800016615). J Thorac Oncol. 2021 May 11:S1556-0864(21)02157-2. doi: 10.1016/j.jtho.2021.04.018. Epub ahead of print. PMID: 33989780.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疗效和安全性#
30
#Oncol#
50
#抑制剂#
38
#美曲塞#
44
#THORAC#
34
#TKI#
43
#培美曲塞#
41
#GFR#
36
#鞘内注射#
40
谢谢梅斯提供这么好的信息,学到很多
64