ESMO 2020:EPI-7386治疗前列腺癌的临床前数据,取得积极结果
2020-09-18 Allan MedSci原创
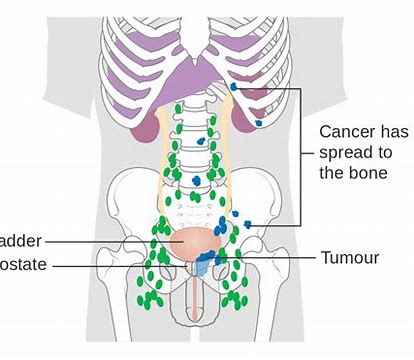
前列腺癌是男性第二大常见癌症,也是全球男性第五大癌症死亡原因。前列腺癌依赖于雄激素来促进肿瘤进展,消耗或阻断雄激素的激素疗法是治疗前列腺癌主要手段。尽管肿瘤最初对降低睾丸激素水平的药物或手术疗法敏感,
前列腺癌是男性第二大常见癌症,也是全球男性第五大癌症死亡原因。前列腺癌依赖于雄激素来促进肿瘤进展,消耗或阻断雄激素的激素疗法是治疗前列腺癌主要手段。尽管肿瘤最初对降低睾丸激素水平的药物或手术疗法敏感,但疾病进展通常是致命的。在过去的五年中,尽管转移性前列腺癌(mCRPC)患者的治疗手段取得了多项进步,但仍需要其他治疗方案来改善患者的临床结局,特别是那些在现有治疗中失败的患者或有禁忌症的患者。
ESSA Pharma是一家临床阶段的制药公司,致力于开发治疗前列腺癌的新型疗法,ESSA Pharma近日宣布,在2020年ESMO虚拟大会上公布的EPI-7386临床前数据取得了积极结果。
EPI-7386是一款第二代N末端域雄激素受体抑制,在体外VCaP模型中,将EPI-7386与enzalutamide,apalutamide或darolutamide的组合治疗比单独使用每种单一药剂对AR相关转录活性的抑制作用更广、更深。
ESSA Pharma总裁兼首席执行官David R. Parkinson说:“这些数据为研究EPI-7386治疗前列腺癌的有效性提供了有力证据”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#EPI-7386#
45
#SMO#
39
#临床前数据#
44
#ESMO#
44
前列腺癌相关研究,学习了,谢谢梅斯
56