Hypertension:ARB和ACEI对COVID-19高血压患者病毒感染、炎症状态和临床结局的影响
2020-05-04 MedSci原创 MedSci原创
这些研究结果支持既往有高血压的COVID-19患者服用ARB/ACEIs。
由于具有诱导ACE2高表达的能力,采用血管紧张素II受体阻滞剂或血管紧张素转化酶抑制剂(ARBs/ACEIs)治疗在促进病毒感染和减少病原性炎症方面可能都存在争议。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员旨在通过一项单中心回顾性研究来评估ARB/ACEI对COVID-19患者的影响。
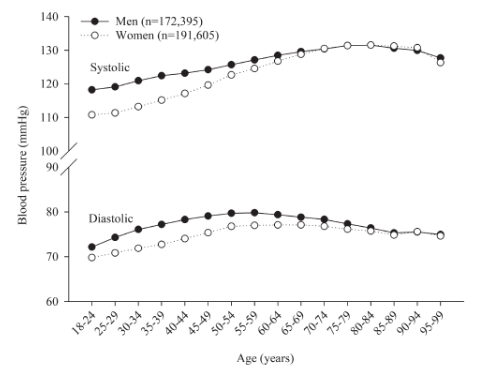
根据他们服用降压药的情况,研究人员将2020年1月5日至2月22日在武汉市湖北省中医院(HPHTCM)住院的126例既往有高血压的COVID-19患者回顾性分为ARBs/ACEIs组(n=43)和非ARBs/ACEIs组(n=83),并随机选择125名年龄和性别匹配的无高血压的COVID-19患者作为非高血压对照者。此外,研究人员还对2019年11月1日至2019年12月31日在COVID-19爆发之前入住HPHTCM的1942名高血压患者的用药史进行了外部比较。研究人员收集,分析和比较了各组流行病学、人口统计学、临床和实验室数据。
在伴有或不伴有COVID-19感染的高血压患者中,使用ARB/ACEI的频率相当。在COVID-19高血压患者中,接受ARB/ACEI或非ARB/ACEI的患者血压相当。但是,ARBs/ACEIs组的CRP(p=0.049)和降钙素原(PCT,p=0.008)的浓度明显较低。此外,与非ARBs/ACEIs组相比,ARBs/ACEIs组的危重患者比例较低(9.3% vs. 22.9%;p=0.061),死亡率较低(4.7% vs. 13.3%;p=0.216)。尽管这些差异未能达到统计意义。
由此可见,这些研究结果支持既往有高血压的COVID-19患者服用ARB/ACEIs。
原始出处:
Guang Yang.et al.Effects Of ARBs And ACEIs On Virus Infection, Inflammatory Status And Clinical Outcomes In COVID-19 Patients With Hypertension: A Single Center Retrospective Study.Hypertension.2020.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.15143
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TENS#
39
#ACE#
43
#炎症状态#
46
#临床结局#
36
#PE#
53
#高血压患者#
28
#Hypertension#
33