FDA优先审评多肽-药物偶联物(PDC)Melflufen治疗难治性多发性骨髓瘤的申请
2020-08-31 Allan MedSci原创
Melflufen对骨髓瘤细胞株表现出细胞毒活性,且该细胞株对包括烷基化剂在内的其他治疗有抵抗力,并且在临床前研究中还显示出Melflufen对DNA修复和血管生成具有抑制作用。
Oncopeptide今日宣布,美国食品药品监督管理局(FDA)已对Melflufen的新药申请进行了优先审查,Melflufen(INN melphalan flufenamide)预计与地塞米松联用治疗对蛋白酶体抑制剂或免疫调节剂或抗CD-38单克隆抗体耐药的多发性骨髓瘤患者(即三级难治性多发性骨髓瘤患者)。这项决定是基于关键性II期研究HORIZON的结果,该研究评估了静脉注射Melflufen与地塞米松联用治疗复发性难治性多发性骨髓瘤(RR MM)患者的有效性和安全性。
Oncopeptides首席执行官Marty J Duvall表示:“这是令人振奋的消息,是Melflufen治疗多发性骨髓瘤患者的重要一步”。

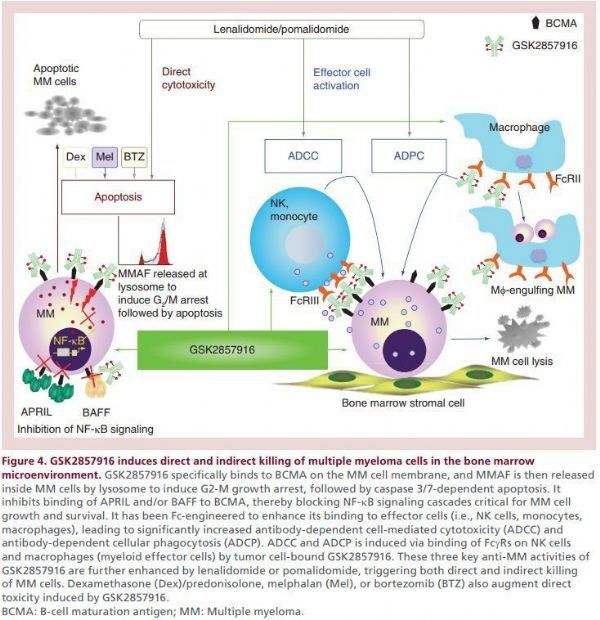
Melflufen(INN melphalan flufenamide)是首创的多肽-药物偶联物(PDC),其能够靶向氨基肽酶并将烷化剂迅速释放到肿瘤细胞中。Melflufen由于其高亲脂性而被骨髓瘤细胞迅速吸收,并立即被肽酶水解,释放出被包裹的亲水性烷化剂负载物。氨基肽酶在肿瘤细胞中过表达,在晚期癌症和高突变负担的肿瘤中更为明显。Melflufen对骨髓瘤细胞株表现出细胞毒活性,且该细胞株对包括烷基化剂在内的其他治疗有抵抗力,并且在临床前研究中还显示出Melflufen对DNA修复和血管生成具有抑制作用。在关键的2期HORIZON研究中,Melflufen+地塞米松治疗复发性难治性多发性骨髓瘤患者的血液学AE和非血液学AE发生率低,显示出令人鼓舞的疗效和临床上可控的安全性。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#优先审评#
35
#pDC#
0
#多发性#
27
#Melflufen#
36
#难治性#
38
#多肽#
37