Circulation:糖酵解解偶联在衰竭心脏恢复过程中的心脏保护作用
2020-08-01 QQY MedSci原创
据报道,部分晚期心力衰竭患者(成为应答者[R])植入左心室辅助装置(LVAD)后机械负荷减轻,心肌结构和功能获得了显著改善。这种治疗策略可能会改变心肌能量代谢,从而逆转衰竭心脏的有害代谢适应。
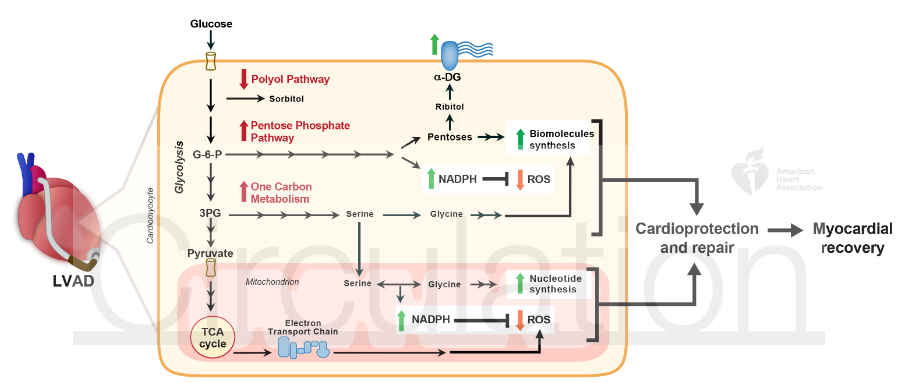
具体而言,Badolia等既往研究证明,LVAD后,心肌细胞中的糖酵解和氧化磷酸化发生解离,其特征是诱导糖酵解后,进一步氧化丙酮酸的三羧酸循环并未增加。造成这种解离的潜在机制尚不清楚。
Badolia等推测,累积的糖酵解中间产物被引导到了心肌保护和修复途径,如磷酸戊糖途径和一碳代谢,这可能介导了应答者的心肌恢复。
Badolia等前瞻性地从LVAD植入前(pre-LVAD)和移植后(post-LVAD)的非心衰患者以及应答者和非应答者中获得配对的左心室心尖心肌组织,进行了蛋白质表达和代谢物分析,并用电子显微镜评估了线粒体的结构。
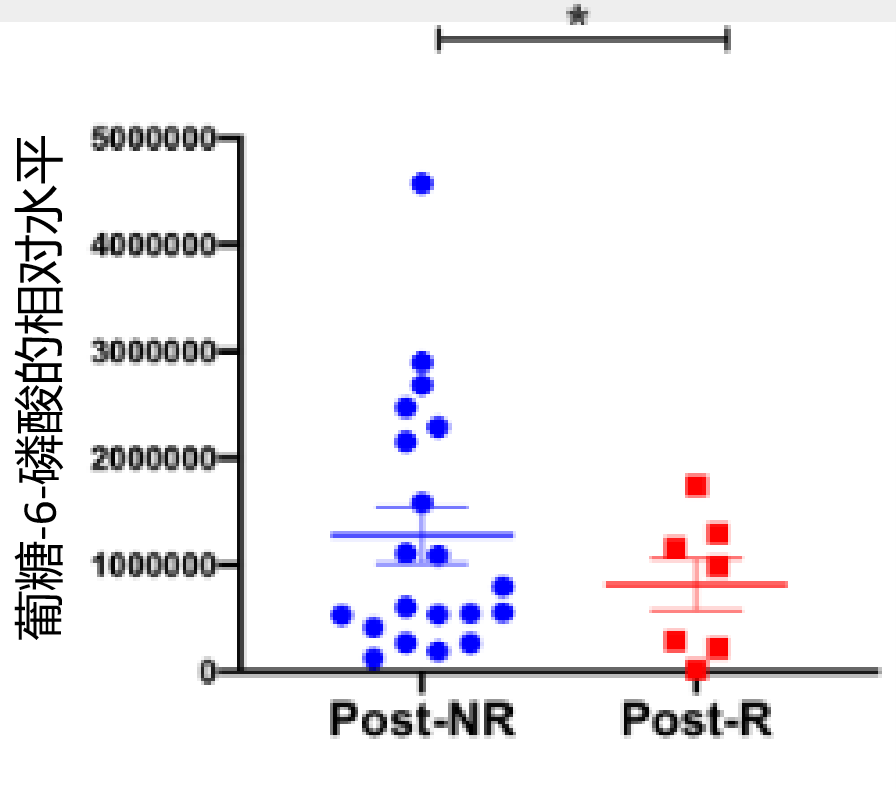
Western blot分析显示,在LVAD后应答者(POST-R)的心肌组织中,磷酸戊糖途径和一碳代谢的限速酶较LVAD后无应答者(PRORD-NR)的显著增加。这些酶的底物,如葡萄-6-磷酸(磷酸戊糖途径)、丝氨酸和甘氨酸(一碳代谢),的代谢产物水平也明显降低。
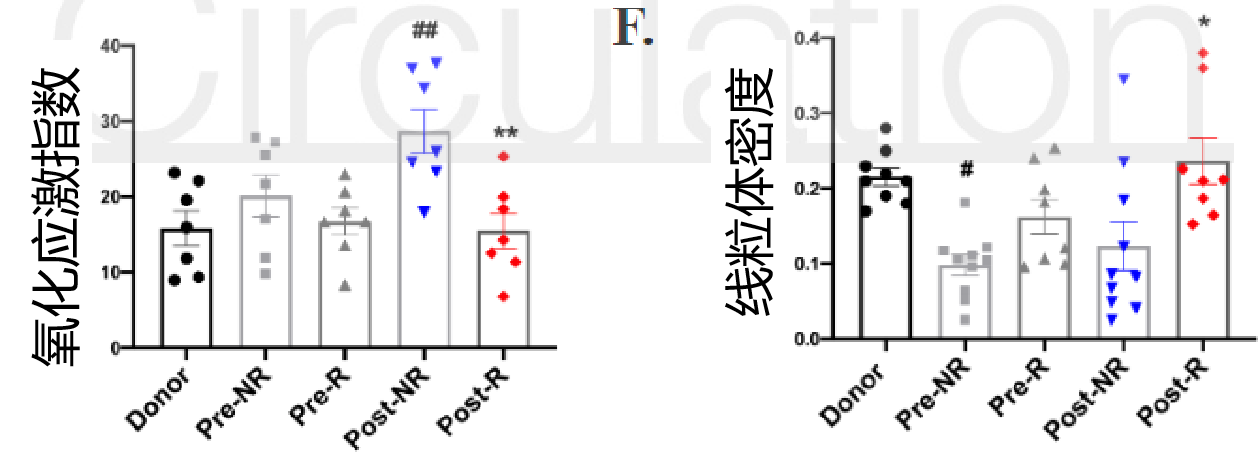
此外,post-R的还原烟酰胺腺嘌呤二核苷酸磷酸水平也显著提高,活性氧水平降低,线粒体密度提高,细胞外基质蛋白α-dystroglan的糖基化增强,所有这些都与在心肌恢复过程中观察到的磷酸戊糖途径和一碳代谢增强相一致。
恢复中的心脏似乎直接将糖酵解代谢产物导入磷酸戊糖途径和1-碳代谢途径,这可能通过产生还原型烟酰胺腺嘌呤二核苷酸磷酸促进生物合成,减轻氧化应激,从而起到心脏保护作用。这些发现为进一步研究衰竭心脏负荷减轻后的恢复过程中的糖酵解诱导的有益效果的机制提供了思路。
原始出处:
Rachit Badolia,et al. The Role of Nonglycolytic Glucose Metabolism in Myocardial Recovery Upon Mechanical Unloading and Circulatory Support in Chronic Heart Failure. Circulation. 2020;142:259–274
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心脏保护作用#
44
#心脏保护#
35
不错的研究方向
0
#糖酵解#
39
#保护作用#
24