肝再生对于肝切除术后肝功能的恢复至关重要。有限的再生能力以及残肝体积不足是肝切除术后肝衰竭的危险因素。尽管炎症在控制肝再生方面发挥着重要作用,但其潜在机制仍不清楚。
近期,附属新华医院移植科顾劲扬主任及上海中医药大学附属曙光医院孔晓妮教授作为共同通讯作者,在Hepatology(IF=17.425)在线发表题为“C-C motif chemokine ligand 5 confines liver regeneration by down-regulating reparative macrophage-derived hepatocyte growth factor in a forkhead boxO 3a–dependent manner”的研究论文。
该研究将CCL5鉴定为肝脏再生的重要负调节因子。
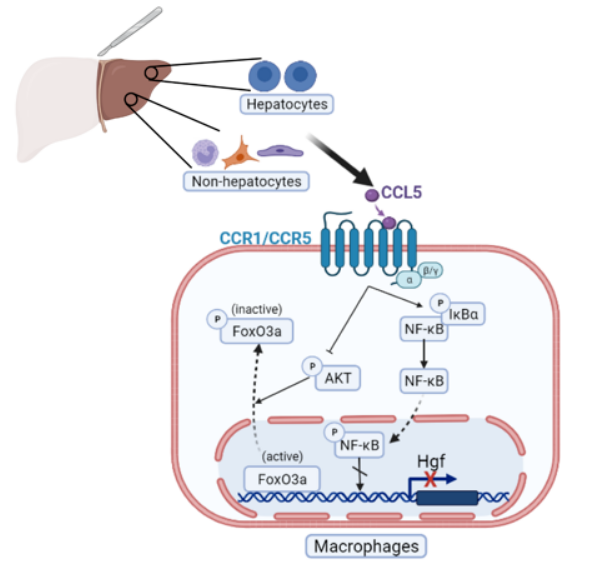
在活体肝移植的健康供体和部分肝切除(PHx)小鼠模型中,CCL5水平明显升高。CCL5敲除小鼠在90%PHx后表现出改善的存活率,并在70%PHx后36小时增强肝再生。然而,与野生型小鼠相比,体外暴露于生长因子的CCL5−/−小鼠的原代肝细胞没有显示出增殖优势。流式细胞术分析显示,在70%PHx后,CCL5−/−小鼠中Ly6Clo巨噬细胞的比例显著增加。RNA测序分析显示,与WT小鼠相比,分选的巨噬细胞(CD11b+Ly6Clo&hi)在CCL5−/−小鼠中表现出增强的修复基因表达。从机制上讲,CCL5诱导巨噬细胞趋向促炎Ly6Chi表型,从而通过CCR1和CCR5介导的FoxO3a途径抑制肝细胞生长因子(HGF)的产生。
最后,在小鼠PHx模型中,CCL5的阻断极大地优化了存活并促进了肝脏再生。
该研究结果表明,通过FoxO3a途径增强修复性巨噬细胞的HGF分泌,抑制CCL5是改善再生恢复的一种有前景的策略,这可能会降低肝切除术后肝衰竭的死亡率。
附属新华医院移植科2019级硕士研究生黄淼、上海中医药大学附属曙光医院2020级博士研究生焦俊喆、附属新华医院移植科蔡浩博士、张亦弛博士以及移植科2020级硕士研究生夏煜寒为文章的共同第一作者。项目受到国家自然科学基金重点项目、面上项目、促进市级医院临床技能与临床创新能力三年行动计划重大临床研究项目、上海杰出青年医学人才、上海市教委高峰高原人才计划等课题资助。
原始出处:
Huang M, Jiao J, Cai H, Zhang Y, Xia Y, Lin J, Shang Z, Qian Y, Wang F, Wu H, Kong X, Gu J.C-C motif chemokine ligand 5 confines liver regeneration by down-regulating reparative macrophage-derived hepatocyte growth factor in a forkhead box O 3a-dependent manner.Hepatology. 2022 Mar 15. doi: 10.1002/hep.32458
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#调节因子#
66
#EPA#
45
#肝脏再生#
47
#CCL5#
43
学习了学习了
0