Plos Med:超60万人研究数据显示,近50%的心血管高危人群血压药物使用不足
2021-03-07 MedSci原创 MedSci原创
尽管高收入国家的心血管疾病(CVD)疾病负担正在下降,但在低收入和中等收入国家(LMIC)的心血管疾病负担正在增加。
尽管高收入国家的心血管疾病(CVD)疾病负担正在下降,但在低收入和中等收入国家(LMIC)的心血管疾病负担正在增加。《中国心血管健康与疾病报告2019》最新数据显示,从1990年~2017年,我国心血管疾病的死亡率总体处于上升阶段,据推算心血管病现患人数3.3亿,此前发布的《中国心血管病报告2018》推算中,全国心血管病患者为2.9亿人。

据数据显示,大约60%的人群发生CVD死亡事件是没有症状的。因此,识别高危人群面临着巨大的挑战,尤其是在医疗队伍技术水平低下、医疗服务不足的情况下。在过去的十年中,人们对CVD的预防工作已经从评估单一的危险因素异常转变为未来发生心血管事件风险进行管理。事实证明该管理方法要优于单一风险因素评估,高风险人群从中获益更多。

近日,发表在Plos Med杂志的一项研究,对2005年至2017年全球45个中低收入国家进行代表性人口调查数据分析,以确定各国具体的CVD风险水平,社会人口统计学因素与CVD风险水平之间的关联以及对WHO降压药物使用指南的遵守情况。
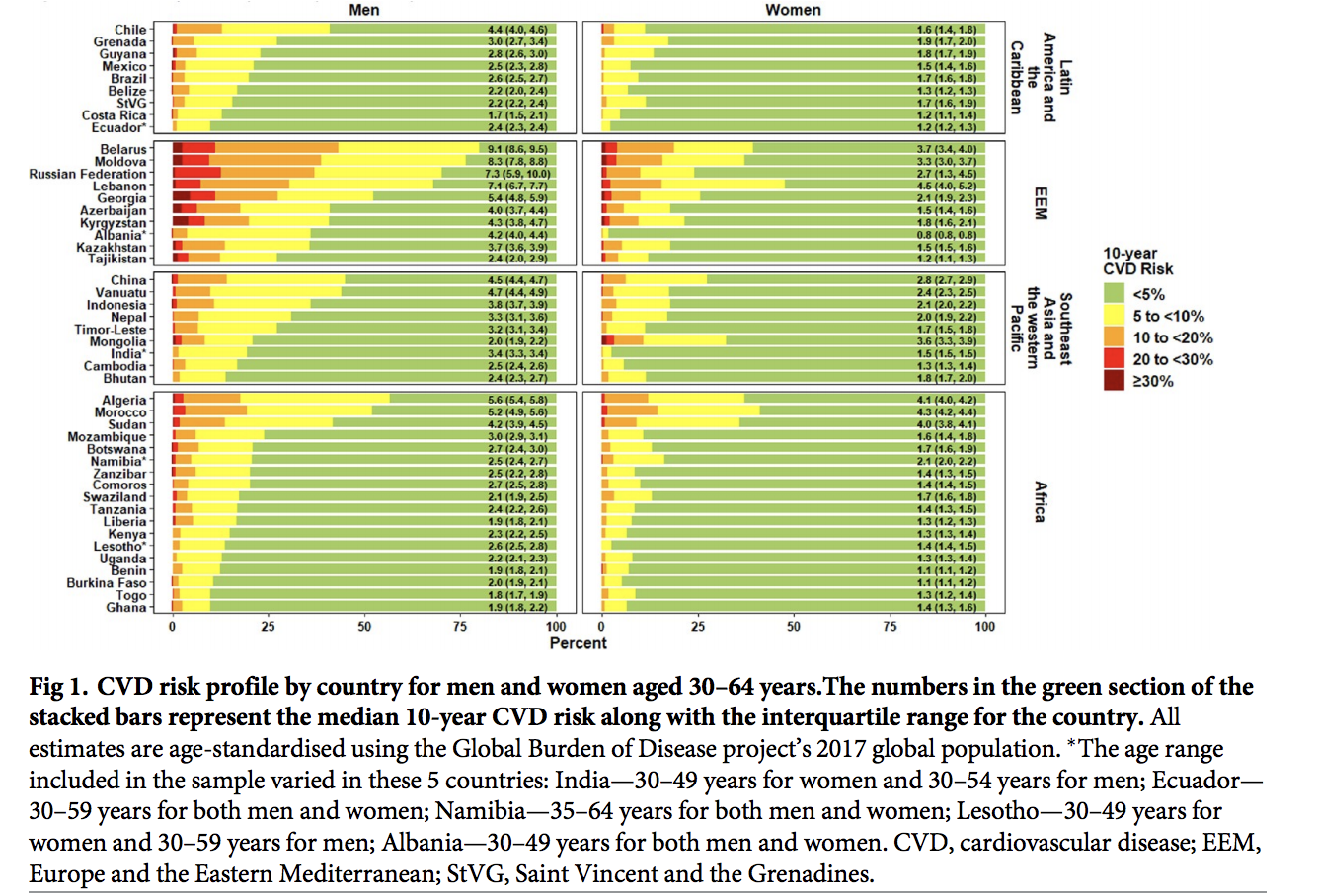
研究人员对来自45个国家的600484名成年人分析发现,男性和女性10年CVD风险中位数分别为2.7%(2.3%-4.2%)和1.6%(1.3%-2.1%),撒哈拉以南非洲地区风险最低,欧洲和东地中海地区风险最高。在大多数国家,较高的教育程度和有工作的人群CVD风险较低。
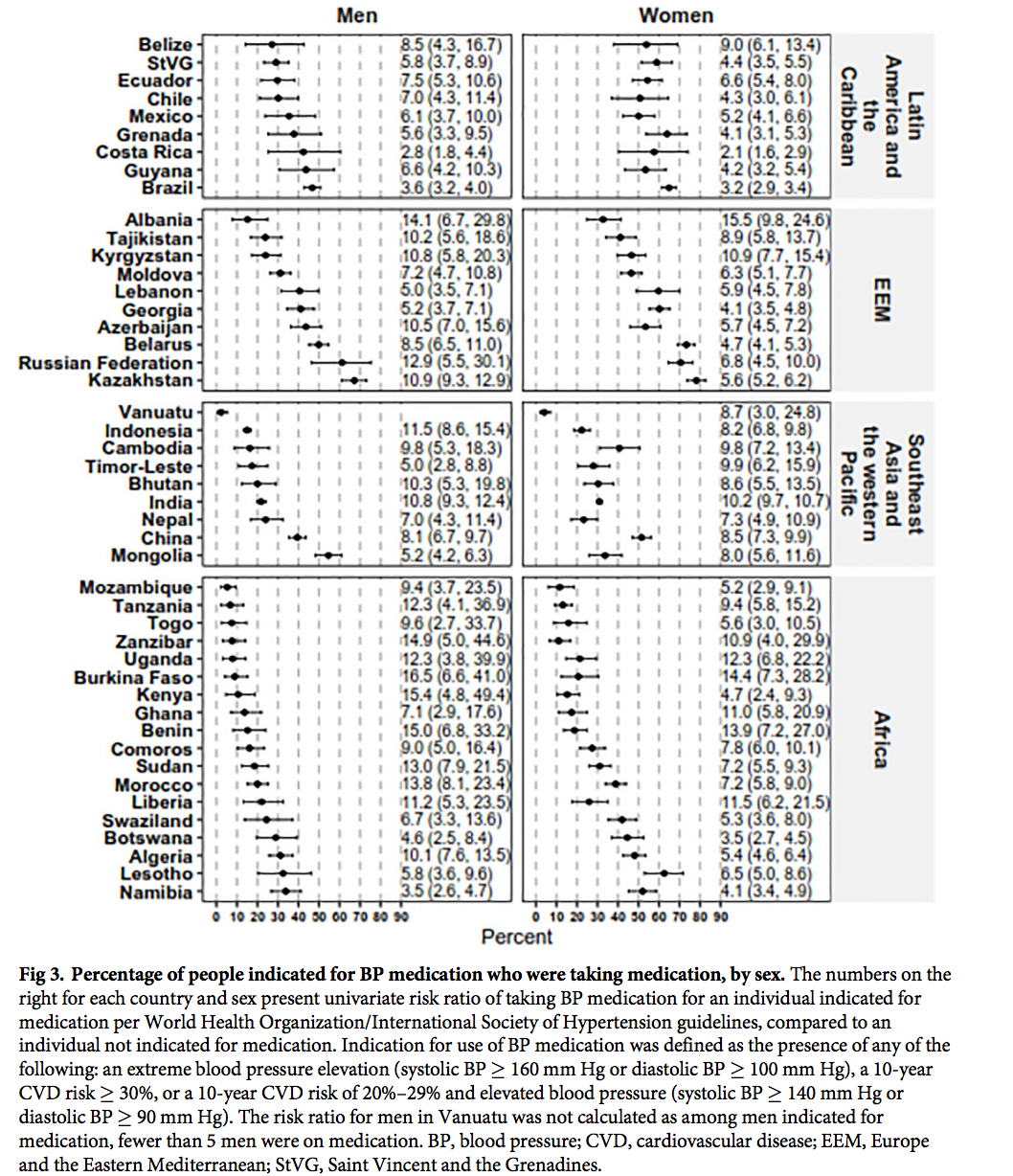
研究人员进一步发现,在所有国家中,CVD风险升高的人药物使用不足,男性服用药物的中位数为24.2%(15.4%-37.2%),女性为41.6%(23.9%-53.8%)。相反,根据CVD风险状态,未服用血压(BP)药物的患者中位数为47.1%(36.1%–58.6%)。在45个研究国家中,大多数国家的BP药物使用与社会人口特征之间没有关联。
综上,各个中低收入国家的CVD风险差异很大,而且在大多数国家中CVD风险与高等教育和就业之间呈反比关系。在所有国家中,CVD风险较低的人群药物滥用,CVD风险较高的人群药物使用不足。本研究结果的巨大异质性也反映了不同国家的情况。需要制定具有针对性的政策,以帮助改善对具有最高CVD风险的人的识别和管理。
原始出处
David Peiris.et al.Cardiovascular disease risk profile and management practices in 45 low-income and middle-income countries: A cross-sectional study of nationally representative individual-level survey data. Plos Med.https://doi.org/10.1371/journal.pmed.1003485
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究数据#
57
#高危人群#
50
#Med#
43
#药物使用#
42
厉害!
89