右侧上颌**磨牙MB2根管1例
2019-02-13 王春芳 马玉 陈亮 牙体牙髓牙周病学杂志
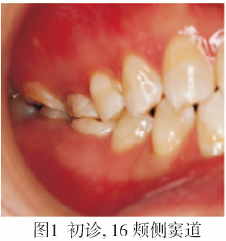
患者女,27岁。因右上后牙咬合疼痛不适数日前来就诊,5年前曾于外院行牙髓治疗。检查:16牙合面大面积龋损、髓腔暴露,探(-),叩(+),不松动,16、17颊侧黏膜见窦道(图1);17残冠,髓腔暴露,根管口可见牙胶样充填物,叩(-),不松动,16、17临床牙冠短。
1.病例报告
患者女,27岁。因右上后牙咬合疼痛不适数日前来就诊,5年前曾于外院行牙髓治疗。检查:16牙合面大面积龋损、髓腔暴露,探(-),叩(+),不松动,16、17颊侧黏膜见窦道(图1);17残冠,髓腔暴露,根管口可见牙胶样充填物,叩(-),不松动,16、17临床牙冠短。
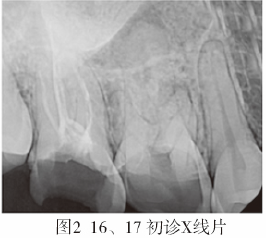
X线片示:16冠部低密度影深达髓腔,根管内未见充填物影像,根尖周稀疏区,近中颊侧隐约可见两根管影像;17根管内充填物影像达根尖,根尖周未见明显异常(图2)。诊断:16慢性根尖周炎;17牙髓治疗后。
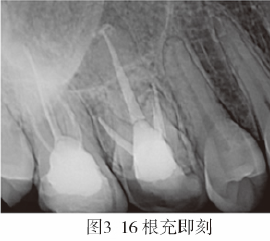
治疗计划:16根管治疗后冠修复;17充填后观察,酌情根管再治疗,择期冠修复。处理:16局麻下开髓,#10K锉探查并疏通根管,未发现MB2;显微镜下ET20去除钙化物,DG16探查发现MB2根管口。疏通根管,冠方预敞,测量工作长度,MB、MB2均为17mm,DB18mm、P19mm。Mtwo机用镍钛器械(VDW,德国)根管预备,52.5g/LNaCLO+170g/LEDTA溶液交替冲洗,超声荡洗,20g/L氯己定溶液终末冲洗,Ca(OH)2封药。两周后复诊,颊侧窦道基本闭合,去除暂封物及根管内Ca(OH)2,超声荡洗,纸尖吸干,AH-Plus+热牙胶垂直加压根充,玻璃离子充填,调牙合(图3)。
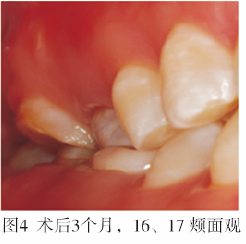
17清理髓腔并备洞,玻璃离子充填,调牙合。3个月后复查,16、17暂封物完好,叩(-),无咬合不适,不松动,颊侧窦道闭合(图4)。
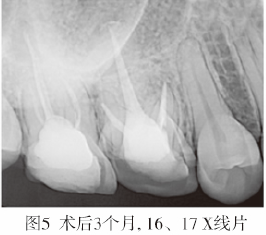
X线片示:16根尖周稀疏区较初诊时有愈合倾向(图5),17未见明显异常。医嘱16、17择期修复治疗,定期复查。
2.讨论
在临床中遗漏根管是根管治疗失败的主要原因之一。因此在治疗时,应仔细探查确定根管数目。上颌第一磨牙MB2的发生率较高,在临床中因医生的技术水平及设备所限经常出现遗漏现象。关于上颌第一磨牙MB2的定位,目前普遍的观点是:MB2根管口多位于MB-P连线的近中舌侧,且在以MB为中心,MB-P为一边,向近中做角度为(22.21±10.35)°的扇形范围内,或是由DB根管口向MB-P连线引一条垂线,两线的交点即为MB2根管口的位置区域(图6)。
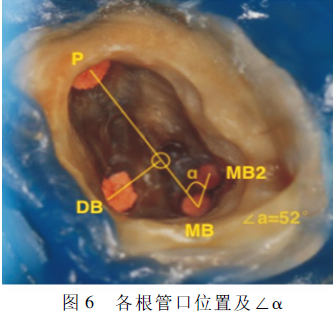
本病例在探查MB2根管口时,发现其位置与上述规律不相符。MB2的开口较常规位置更偏近中偏颊侧,在该病例中,治疗初始借助根管显微镜按照上述规律探查MB2,在可能存在MB2的范围内均未发现其根管迹象,但术前X线片提示我们该病例存在MB2,术者根据髓底、钙化物及正常牙本质壁颜色的差别,借助超声设备去除钙化物,最终确定MB2根管口的位置。该病例中MB2的位置较常规更偏近中偏颊侧,同时∠α为52°,远大于李健等报道的最大值32.56°(图6)。MB根管因受到龋损、修复体等长期刺激后,导致MB2根管口缩小或完全被钙化,从而增加其定位的困难。
根管显微镜因具有良好的光源和足够大的放大倍数,能区分髓底牙本质在颜色和质地方面的细微变化。配合不同型号的超声工作尖,可准确去除髓腔及连接各根管口间窄沟内的钙化物,从而提高MB2的定位率。
近年来,锥形束CT(corn beam computed tomography,CBCT)在牙髓治疗中的应用越来越广泛。Nur等的研究表明,CBCT在上颌第一磨牙MB2检测中具有较高的价值。CBCT的三维显像可以较为清晰的展现MB2根管系统,利于寻找和定位MB2。因此,对于疑难病例术者可先行CBCT确定根管的数目及根管口的位置后,再于口腔科手术显微镜下有目的和方向的探寻根管口。
结合本病例,术者在常规可能出现MB2的范围内未发现MB2时,可以在征得患者同意后,借助CBCT确定MB2根管口的位置后结合根管显微镜和超声设备进一步探寻,从而提高探寻的准确性,同时也降低盲目操作的风险。该病例提示,在临床中我们应该充分利用现有的设备与技术条件,不断提高治疗成功率。
原始出处:
王春芳,马玉,陈亮.右侧上颌第一磨牙MB2根管1例[J].牙体牙髓牙周病学杂志,2018,28(01):58-59.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#MB2#
57
#根管#
32
#磨牙#
30
#上颌#
44