Allergy Asthma Immunol Res:特应性皮炎、哮喘和过敏性鼻炎患者的生活质量和心理健康状况如何?
2022-04-11 AlexYang MedSci原创
近日,来自韩国天主教大学的研究人员调查了过敏性疾病患者与非过敏性对照组人群的心理健康状况和生活质量。相关研究结果发表在Allergy Asthma Immunol Res期刊上。
近日,来自韩国天主教大学的研究人员调查了过敏性疾病患者与非过敏性对照组人群的心理健康状况和生活质量。相关研究结果发表在Allergy Asthma Immunol Res期刊上。

本研究采用2016年至2018年韩国全国健康与营养调查的全国性、基于人口的横断面数据。研究使用倾向性匹配得分来平衡过敏性疾病组和相应对照组之间的年龄和性别分布。特应性皮炎(n = 446)和哮喘(n = 483)组与对照组按1:10的比例进行比较,过敏性鼻炎(n = 2357)组与对照组按1:2的比例进行比较。研究人员使用多重逻辑回归分析来评估基于过敏性疾病存在的心理健康状况和健康相关生活质量(HRQoL)的几率(ORs)。
结果显示,调整混杂因素后,哮喘组(OR,1.41,1.83和2.1)和过敏性鼻炎组(OR,1.35,1.48和1.83)与非过敏性对照组相比,严重心理压力、心理咨询和抑郁症诊断的OR显著增加。与对照组相比,哮喘组的活动能力出现严重问题的比率有更明显的增加。
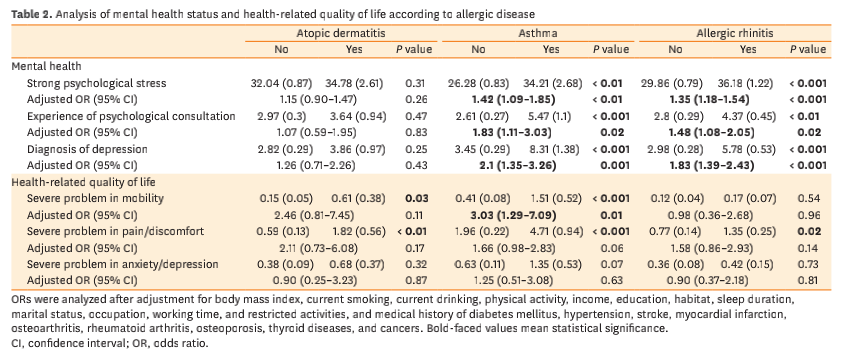 图1 过敏性疾病患者心理健康状况及健康相关生活质量分析
图1 过敏性疾病患者心理健康状况及健康相关生活质量分析
因此,研究人员认为应努力管理特应性皮炎、哮喘和过敏性鼻炎患者心理问题,改善的他们的HRQoL。
原始出处:
Lee GN, Koo HYR, Han K, et al. Analysis of Quality of Life and Mental Health in Patients With Atopic Dermatitis, Asthma and Allergic Rhinitis Using a Nation-wide Database, KNHANES VII. Allergy Asthma Immunol Res. 2022 Mar;14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#过敏性#
65
#AST#
43
#asthma#
57
学习了
67
学习了,谢谢分享
72
#ALL#
41
#健康状况#
49