Br J Cancer:SLC38A4调控Wnt/β-catenin/MYC/HMGCS2信号通路抑制肝细胞癌的发生发展
2021-07-24 xiaozeng MedSci原创
肝癌作为全球第六大常见癌症,也是全球癌症相关死亡的第三大原因。
肝癌作为全球第六大常见癌症,也是全球癌症相关死亡的第三大原因。在所有恶性肿瘤中,肝癌的预后相对较差,患者的5年生存率<20%。肝细胞癌(HCC)是肝癌的主要组织学亚型。目前急需进一步的研究驱动HCC发生发展的关键分子机制。
越来越多的证据显示,HCC与胚胎肝脏发育具有许多共同的分子特征。这些共同的分子事件被视为癌胚分子事件,例如胎儿肝脏和HCC中甲胎蛋白(AFP)的高表达。此外,一些具有更强胚胎基因表达特征的HCC的预后更差。
因此,进一步揭示胎儿肝脏发育和HCC期间的关键癌胚事件将为HCC发生和治疗靶点的研究提供新的见解。
在该研究中,研究人员通过qRT-PCR、蛋白质印迹、TCGA和GEO数据集研究了SLC38A4和HMGCS2的表达水平和临床相关性,并通过功能测定研究了SLC38A4的生物学作用。
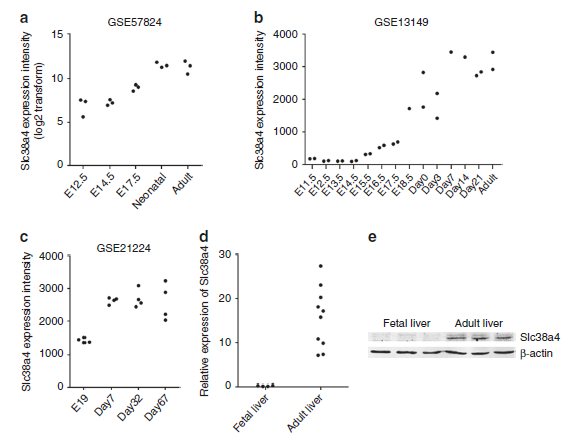
研究人员将SLC38A4的沉默确定为癌胚分子事件。DNA高甲基化会导致胎儿肝脏和HCC中Slc38a4/SLC38A4的表达下调。研究人员发现,SLC38A4的低表达与HCC患者的不良预后相关。
相比于成人,胎儿肝脏中Slc38a4的表达下调
功能研究显示,敲除SLC38A4能够促进HCC细胞的增殖、干细胞特性和迁移能力,抑制体外HCC细胞的凋亡,并进一步抑制体内HCC肿瘤的发生。
HMGCS2被鉴定为SLC38A4的关键下游靶标。SLC38A4可通过上调AXIN1的表达以及抑制Wnt/β-catenin/MYC信号通路来提高HMGCS2的表达水平。功能性拯救(rescue)试验显示,过表达HMGCS2能够逆转SLC38A4敲除在HCC中的致癌作用。
在HCC组织中SLC38A4的表达下调且与患者的预后呈负相关
总而言之,该研究结果显示,SLC38A4的表达下调被认为是一种新的癌胚事件,SLC38A4也被鉴定为HCC发生发展过程中的一种新型肿瘤抑制因子。
原始出处:
Li, J., Li, Mh., Wang, Tt. et al. SLC38A4 functions as a tumour suppressor in hepatocellular carcinoma through modulating Wnt/β-catenin/MYC/HMGCS2 axis. Br J Cancer (17 July 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#肝细胞#
35
#细胞癌#
44
#发生发展#
42
#MYC#
51
#信号通路#
40
#WNT#
39