JAMA Cardiol:4级肺栓塞临床概率评分(4PEPS)在减少肺栓塞过度影像学检查方面的应用
2021-03-04 MedSci原创 MedSci原创
在减少影像学检查方面,4PEPS策略比之前提出的所有策略表现更好。
肺栓塞(PE)的诊断在过去的几十年里取得了重大的进展,基于临床概率评估、D -二聚体测试和肺血管CT造影(CTPA)的标准诊断策略被证明失败率非常的低。目前,对于疑似PE的CTPA检查在临床上有很大的增加。确切的原因包括D -二聚体检测缺乏特异性,有很大比例的患者出现假阳性,最终还是需要影像学排除PE。且CTPA很容易获得,快速,微创,比通气/灌注(V/Q)扫描更敏感。
pixabay.com
然而,有研究结果观察到,虽然PE诊断率的轻微增加,但在患者最终结果方面没有表现出明显的好处,特别是与PE相关的死亡率。其中一种解释是,由于进行了更多的CTPA检查,出现假阳性结果或非临床相关诊断的风险更大。此外,CTPA使患者面临过敏、肾衰竭和累积辐射致癌的风险。
因此,人们提出了几种策略来减少PE的过度检测和过度诊断(表1)。这些策略在安全性和有效性方面被证明是令人满意的,但它们基于不同的评估临床前检测概率的方法,因此很难将它们结合起来,也增加了临床实践中误用的风险。
基于此,有研究者开发和验证了一个预测试概率评分——4级肺栓塞临床概率评分(4PEPS),通过整合所有先前提出的策略来减少影像学检查。并回顾性评估基于这一新评分的诊断策略的安全性及其在减少影像学检查方面的有效性。该研究结果近日发表在JAMA Cardiology杂志上。
这项研究包括来自美国和欧洲急诊科怀疑有PE的门诊病人。3个合并管理研究的个体数据(n=11114;PE总患病率,11%)用于衍生队列和内部验证队列。外部验证队列来自2个独立研究,第一个是高PE患病率(n=1548;患病率,21.5%),第二个是中等PE患病率(n=1669;患病率,11.7%)。数据收集时间为2003年1月至2016年4月,数据分析时间为2018年6月至2019年8月。主要结果和测量指标为:在初次检查或随访期间确诊PE的比率和影像学检查的比率。
研究结果显示,在5588名衍生队列患者中,3441名(61.8%)为女性,平均年龄为52岁(18.5岁)。4PEPS包括13个临床变量,得分从2到5。结果如下:(1)4PEPS小于0时PE发生率很低:未经检测就排除PE诊断;(2)4PEPS为0~5时PE发生率很低:D-二聚体含量小于1.0μg/mL时PE排除;(3) 如果4PEPS为6-12,则PE发生的可能性中等:如果D-二聚体水平低于年龄调整的临界值,则PE排除;如果4PEPS大于12,则PE发生的可能性高:未经D-二聚体检测,通过成像排除PE。在第一个和第二个外部验证队列中,接受者-操作者特征曲线下面积分别为0.79(95%CI,0.76-0.82)和0.78(95%CI,0.74-0.81)。采用4PEPS策略的假阴性检出率分别为0.71%(95%CI,0.37~1.23)和0.89%(95%CI,0.53~1.49)。在第一个和第二个外部验证队列中,影像学检查的绝对减少率分别为22%(95%CI,26-19)和19%(95%CI,22-16)。在成像测试方面,4PEPS策略与所有最近的策略相比都是有利的。
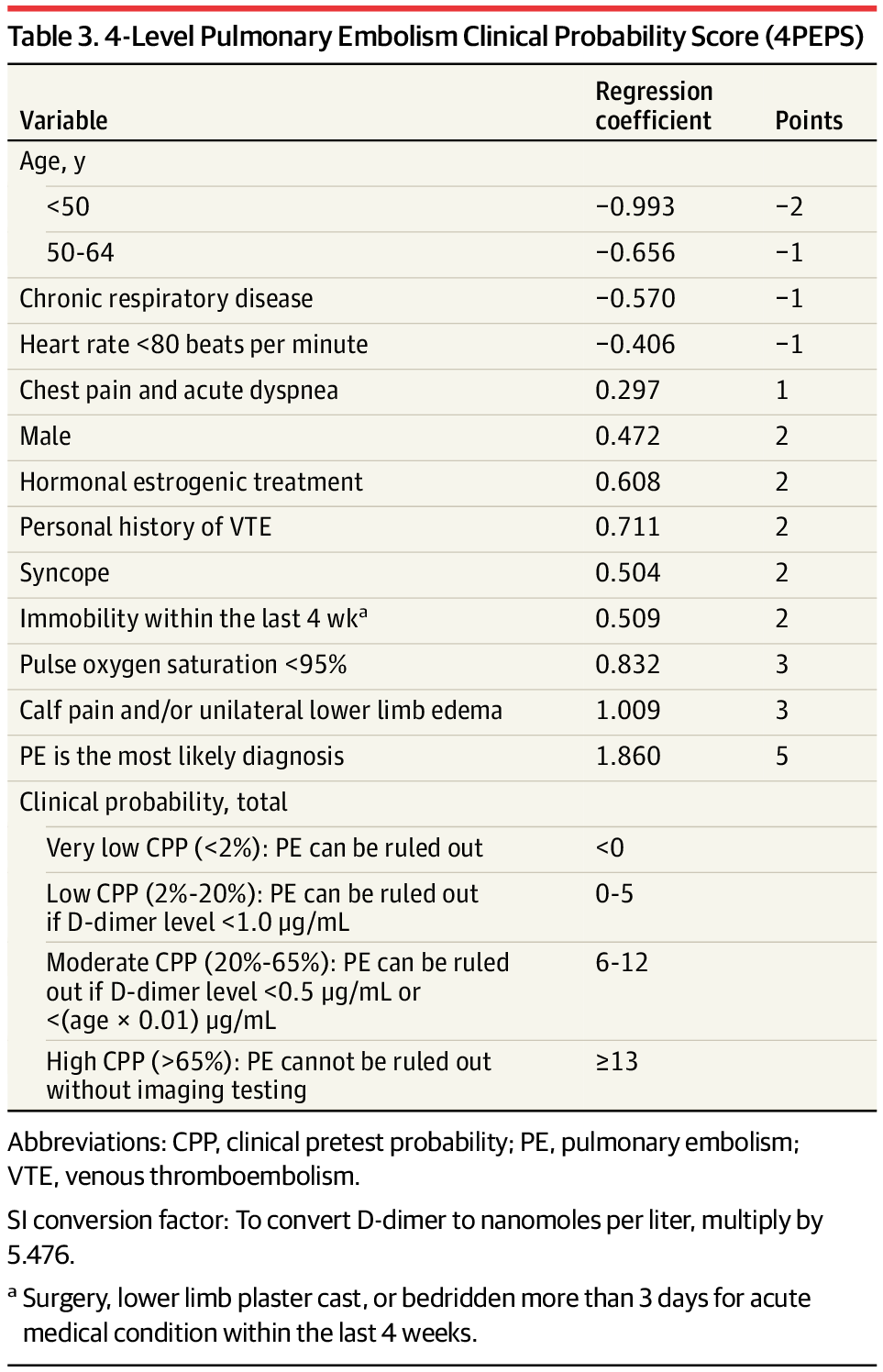
4级肺栓塞临床概率评分(4PEPS)

根据回顾性应用的策略进行诊断性试验和假阴性试验
回顾性地将4PEPS诊断策略应用于2个外部验证队列,假阴性检测率低于1%,在减少影像学检查方面,4PEPS策略比之前提出的所有策略表现更好。总之,使用贝叶斯方法,研究者得到了一个新的4级临床概率评分(4PEPS),以帮助E医生对疑似PE患者做出决定。
4PEPS策略的准确性、安全性和有效性在两个独立的外部验证队列中得到了证实,一个是中度PE患病率,另一个是高PE患病率。在这两个队列中,使用4PEPS可以降低诊断失败率,大幅减少影像学检查。现在应该在正式的结果研究中进行测试。
参考文献:Roy P, Friou E, Germeau B, et al. Derivation and Validation of a 4-Level Clinical Pretest Probability Score for Suspected Pulmonary Embolism to Safely Decrease Imaging Testing. JAMA Cardiol. Published online March 03, 2021. doi:10.1001/jamacardio.2021.0064
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EPS#
38
#Cardiol#
40
#临床概率#
40
赞一个,非常不错!
61
#PE#
40
好文章
79
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
61
认真学习
87
好文章!
90
学习了
66