Haematologica:RXRA的突变重新引起了对类视黄醇治疗急性髓系白血病的兴趣
2022-08-29 MedSci原创 MedSci原创
最近的两项研究重新唤起了人们对 AML 中 RXRA 信号传导的兴趣。

对于急性髓性白血病 (AML) 治疗而言,“一刀切”的想法显然已经过时:未来的治疗将取决于表型或基因定义的亚型。最引人注目的例子是由 PMLRARA 融合蛋白驱动的急性早幼粒细胞白血病 (APL)。在 APL 中,一种占 AML 病例 5% 的亚型,两种靶向药物的组合,全反式维甲酸 (ATRA) 和三氧化二砷通过PML-RARA驱动程序降解、分化和恢复治愈了超过 90% 的患者PML 依赖性衰老。这些临床成功促使人们尝试利用类视黄醇治疗其他癌症。不幸的是,仅 ATRA 治疗在大多数非 APL AML 中效果不佳。
维甲酸信号传导很复杂,现在仍不完全清楚。ATRA 主要通过与维甲酸 X 受体 (RXR) 组装的维甲酸受体 (RAR) 的异二聚体复合物起作用。这些 RXR 是许多 II 类核受体的关键异二聚化伙伴,可能是配体依赖性转录因子或沉默受体,允许序列特异性 DNA 识别。因此,RXR 的治疗靶向可能是一种在 RXR/RAR 转录复合物控制下激活靶点的策略。然而,原则上,RXR/RAR 信号不能单独被 RXR 配体激活,至少部分是因为共阻遏物仍然与 RAR 牢固结合。这可以由其他信号级联/第二信使调制,例如 cAMP。
在 AML 中,这种观点受到了挑战。RXR 配体(rexinoids,如贝沙罗汀)可能在体外和体内发挥一些差异化作用。造血细胞和一些 AML 表达了内源性 RXRA 配体。最近的两项研究重新唤起了人们对 AML 中 RXRA 信号传导的兴趣。
第一个表明,在由 KMT2A-MLLT3 驱动的 AML 中,rexinoids 部分抑制了 AML 生长并引发了分化。此外,RXR 的基因消融加速了 AML 的生长,而 RXRA 和 RARA 的伴随激活促进了分化或细胞凋亡。希望这些关键调节剂的双重激活可以在 AML 中更有效地利用类视黄醇。
在去年发表于Haematologica的第二项研究中,di Martino等报告了一个偶然发现的 RXRA (RXRA DT448/9PP) 激活突变,它有效地激活 rexinoid/retinoid 下游信号并足以诱导 KMT2A-MLLT3 转化细胞的终末分化。RXRA 的 C 末端螺旋 12 或 AF-2 螺旋是通过控制共激活因子/共抑制因子结合来决定配体依赖性转录活性的关键因素。
令人惊讶的是,di Martino等人证明 RXRA DT448/9PP 过表达导致转录活性增强,导致 KMT2AMLLT3 转化的 AML 细胞中的多种分化特征,特别是集落形成能力的丧失。这种组成型活性 RXRA 变体完全独立于配体结合共激活剂。因此,不能分别通过 RXR 或其他核受体的选择性拮抗剂或它们的激动剂来消除或进一步促进反式激活。
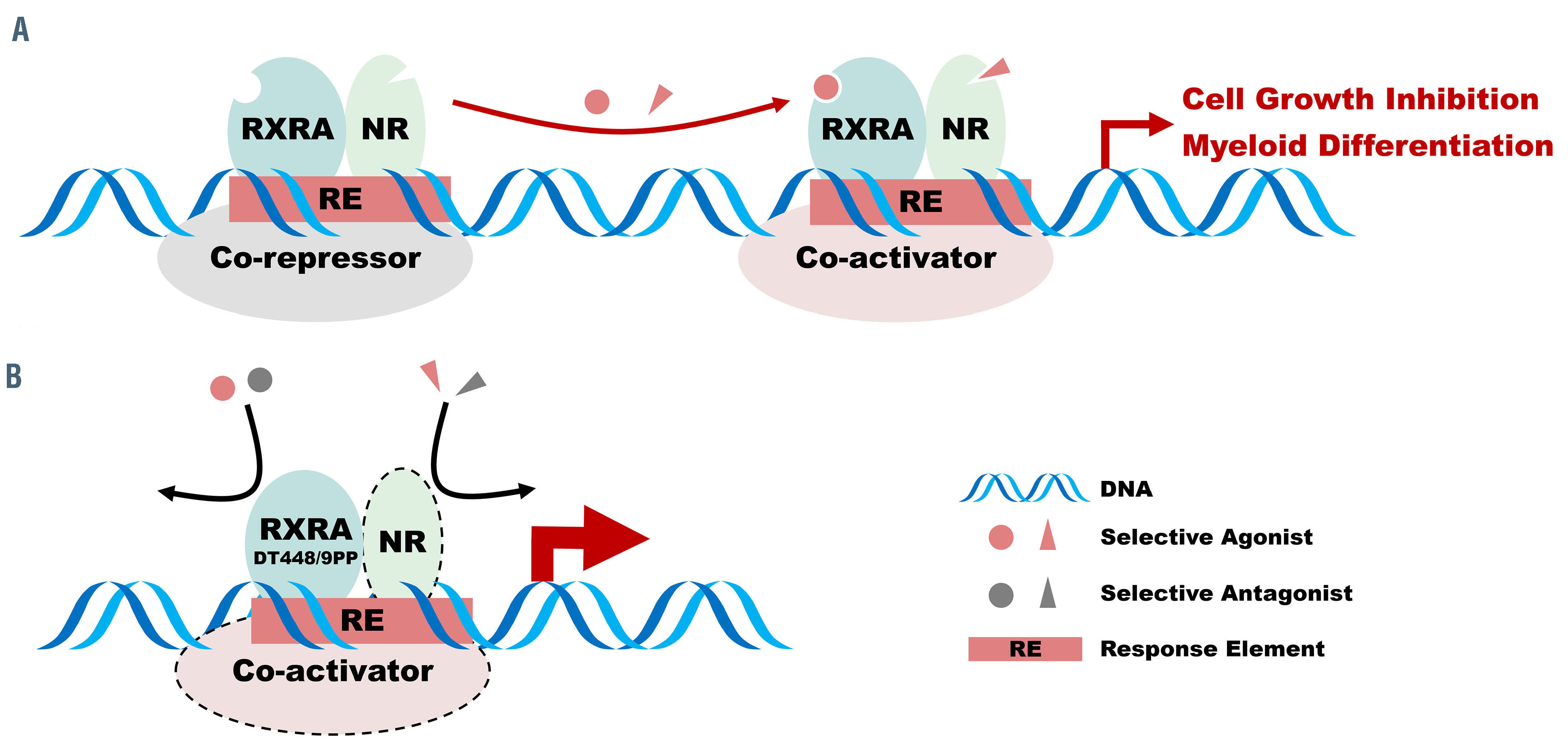
图 :组成型活性 RXRA DT448/9PP 效果的示意图总结。(A) 在正常情况下,RXRA 与包括 RARA 在内的其他核受体 (NR) 异二聚化的转录活性由于共阻遏物结合而保持沉默。选择性激动剂激活 RXRA/NR 驱动的转录,导致细胞分化和生长停滞。(B) RXRA 中残基 488/9 的突变允许有效的配体非依赖性转录激活并驱动分化。
这些有趣的观察表明,即使 rexinoids 和 retinoids 对这些 AML的骨髓分化产生协同作用, RXRA 的更深刻的“非常规”激活可以启动终末分化,这种主要的转录调控复合物值得进一步研究以破译它如何在没有配体的情况下变得如此有效,未来的研究应该确定哪种 AML 对 RXRA 信号表现出这种高度的敏感性。在非 APL AML 中出现的类视黄醇敏感性在联合治疗的情况下尤其重要。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#髓系白血病#
57
#HAE#
52
新的靶点
68
棒
82
学习
82
#EMA#
36
#视黄醇#
54